Experiencing a headache every once in a while isn’t something to worry about. Most people suffer from pain in the face and neck because of factors such as occasional stress and lack of sleep. However, when your headaches become recurring or chronic, there is no time to lose. Understanding what’s causing them and finding the right line of treatment are essential steps toward regaining control over your life.
NextPain Care’s innovative 3-level system, focusing on a holistic approach, can help you address the root cause of the pain behind your headaches. This system starts with conservative treatments, progresses to medications if needed, and utilizes advanced procedures for more severe cases. Ultimately, this approach can help you restore your health and functionality. Discover how in the guide below.
Recurring Migraines
Migraines are a type of headache that affects one side of the head, with painful sensations usually affecting the forehead and the areas around the eye. The pain can spread through the head and the scalp, and it can be accompanied by a range of symptoms, including nausea, vomiting, and sensitivity to stimuli such as light, odors, and sounds.
Migraines can be either episodic or chronic:
- Episodic migraine: 0-14 days of headache per month
- Chronic migraine: 15 or more headache days per month
The frequency and intensity of migraine attacks can vary over time. You may be diagnosed with episodic migraine at first, but your condition can develop into chronic headaches over time. Conversely, chronic migraines can reverse back into episodic headaches due to health events or aging.
In the sections below, we’ll look at the symptoms, nature, and impact of migraine.
Typical Symptoms
Each migraine is unique in terms of symptom intensity and nature. These headaches tend to develop in four distinct phases:
- Prodrome: This “pre-headache” phase occurs between three days and 24 hours before a migraine attack. Prodrome symptoms include food cravings, neck stiffness, abnormal sensations, hyperactivity, fatigue, and excessive yawning. Recognizing these symptoms early can help you intervene to reduce the intensity or duration of a migraine attack. You can do so by avoiding triggers, resting, and reducing tension.
- Aura: The aura phase indicates that a migraine attack is around the corner. Aura symptoms tend to occur within 24 hours before the headache and intensify 10 – 60 minutes before the attack. These symptoms vary from one person to another and include visual disturbances (e.g., flashes of lights, tunnel vision, vision loss, and even hallucinations), sensor and motor disturbances, and speech issues, such as slurred speech.
- Migraine attack: This phase is characterized by headache as well as nausea, vomiting, and hypersensitivity to light and sound. We’ll look at these symptoms in more detail below. The headache phase of a migraine attack can last between four and 72 hours.
- Postdrome: Postdrome, also known as “migraine hangover,” occurs in the 24 – 48 hours after a migraine attack has subsided. In this phase, you may experience fatigue, muscle or joint soreness, brain fog, and lack of focus.
While only around a third of people with migraines have premonitory symptoms such as prodrome or aura before a headache, most symptoms of a migraine attack are similar among patients with this condition. These symptoms include:
- Pain, usually localized to one side of the head
- Painful sensations that spread across the scalp, face, and neck
- Nausea and vomiting
- Sensitivity to light, odors, and sounds
- Cognitive difficulties, trouble concentrating, lack of focus, and brain fog
- Extreme fatigue (often aggravated by nausea, vomiting, and pain)
- Changes in body temperature
- Paleness
- Diarrhea
- Blurred vision
- Phantom smells
While these symptoms should start to subside within a few hours of the beginning of the attack, it is important to seek immediate medical attention if your symptoms last longer than two days or if they are accompanied by numbness, nosebleeds, vision loss, high fever, chest pain, or shortness of breath. These symptoms may indicate a medical emergency, such as a stroke.
Distinguishing Between Migraines And Common Headaches
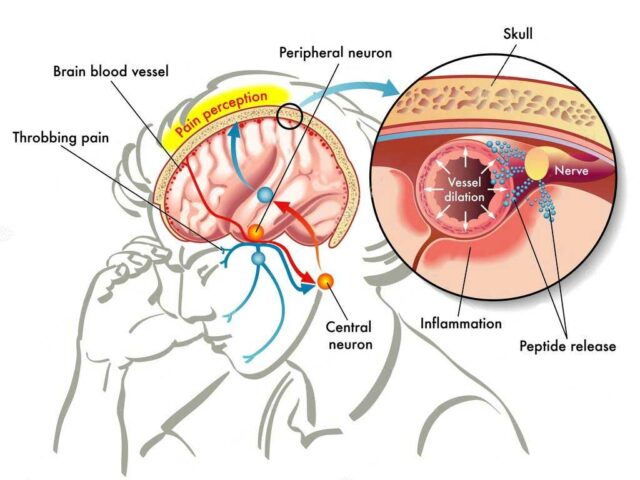
When looking at the official classification of headache disorders, migraines are considered to be primary headaches. Primary headaches are the ones that don’t have another underlying cause. In other words, the pain itself is the condition. However, new research has highlighted how migraines are, in fact, a neurological disorder that occurs due to changes in the sensory pathways, blood flow, and chemical reactions in the brain. These changes cause abnormal waves of activity among groups of excitable cells.
This peculiarity is what causes people with migraines to experience symptoms such as nausea, vomiting, and reduced cognitive capabilities. There are also signs and symptoms that will set a migraine apart from a normal headache (i.e., tension headache):
- The presence of premonitory signs, such as prodrome or aura syndromes
- Sensory, motor, and speech changes
- Inflammation, which leads to an upset gut, as well as sensitivity to light, odors, or sounds
If you are unsure about the type of headache you are experiencing, obtaining an accurate diagnosis is the first step to finding the best line of treatment for your needs.
Migraine Prevalence And Its Impact On Daily Life
Occasional headaches affect over half of the world’s population, while nearly a billion people worldwide (39 million in the US) suffer from migraines. According to the Centers for Disease Control and Prevention (CDC), approximately 25% of adults aged between 18 and 44 suffer at least one severe headache or migraine every three months.
In terms of the impact that migraines have on a person’s life, this condition can bring on a whole host of complications. For example, patients with migraines tend to miss, on average, 4.4 days of work a year due to pain, and they live with a further 11 days of reduced productivity annually. When looking at the financial burden of migraine, patients with this condition report facing annual medical costs as high as $9,500 to manage their chronic pain.
Other complications, which we will examine in more detail below, include sleep disturbances, a higher risk of mental health conditions, and cognitive disorders such as dementia.
It has been seen that around a quarter of chronic migraine cases will go into remission and become episodic, which makes them far easier to manage. Nonetheless, you should not have to endure years of pain and life-limiting symptoms. Finding an adequate treatment plan can help you regain control over your life and support the earlier remission of migraines.
What Causes Migraines In Individuals?
If you have been diagnosed with a migraine disorder, headache attacks can develop after exposure to certain triggers. The most common triggers include:
- Hormonal changes (specifically the fluctuations of estrogen that occur during events such as pregnancy and menstruation)
- Certain pharmaceuticals
- Drinking alcohol
- High-stress levels
- Skipping meals
- Sleep deprivation
- Caffeine
- Environmental factors such as certain foods, flashing lights, and strong odors
It is important to understand that these triggers may start a migraine attack, but they are not the root cause of migraine disorders. To this day, the real causes of migraine aren’t well understood. However, research has shown that a role is played by genetic factors, neurological aspects, medical conditions, and environmental and lifestyle influences.
In the sections below, we’ll look at these aspects in more detail.
Genetics’ Role
Genetics have been seen to be a critical factor in 34-64% of migraine cases. However, understanding how genetics influence the risk of developing a migraine disorder isn’t always straightforward.
According to studies, patients with a first-degree relative with migraine (such as a parent or sibling) are twice as likely to develop this disorder. The reason for this is that genes influence how sensitive people are to changes in the environment and known migraine triggers.
What’s more, a 2023 review shows that hereditary small-vessel disorders can increase the risk of developing migraines. The same study also reports that there are shared genetic factors between migraines and conditions such as depression and high blood pressure. This means that a patient at risk of migraine disorders is also at greater risk of developing these comorbidities.
The Influence Of Hormones On Migraines
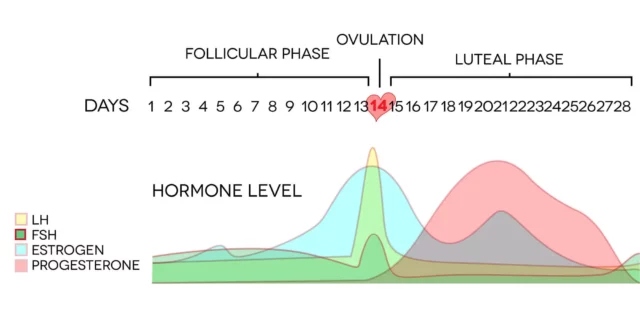
Women are two to three times more likely than men to develop migraines. One of the main reasons for this is that females experience significant fluctuations in estrogen levels during their lifetimes.
Estrogen is a hormone responsible for enabling and regulating the female reproductive system. While the link between changes in estrogen levels and migraines isn’t fully understood, research has shown that there are mechanisms that can lead to migraine headaches:
- Estrogen can affect the action of serotonin, a neurotransmitter (a chemical messenger) that influences mood and pain perception.
- Estrogen can cause changes in blood pressure and blood vessels, which have been seen to play a role in migraines.
Estrogen fluctuations can occur due to a wide range of factors, including:
- Using birth control (hormonal) pharmaceuticals
- Perimenopause
- Menopause
- Pregnancy
- Menstruation
- Hormone replacement therapy
- Hysterectomy
- Gender-affirming surgeries
- Pregnancy
- Childbirth
During these health events, estrogen can suddenly spike or drop, which can lead to the development of a migraine disorder. It has been seen that many women experience menstrual migraines in the days leading up to menstruation, or within three days after the period starts.
Some of the most influential events associated with migraines include pregnancy and perimenopause.
Pregnancy
Migraine headaches are a common type of headache during pregnancy, alongside tension headaches. If you have been diagnosed with a migraine disorder, you are likely to notice an increase in the intensity and frequency of attacks during the first trimester due to the quickly rising levels of estrogen and the expansion of blood vessels in the brain (due to changes in serotonin levels).
After the third month of pregnancy, these headaches tend to ease down and become less frequent, but you may experience a new onset aura during the second and third trimesters.
Perimenopause And Menopause
Perimenopause is a transitioning period leading up to menopause. It usually occurs in the months or years before your last period. During perimenopause, you are likely to experience spiking and dropping estrogen levels, which are accompanied by symptoms such as high-stress levels, anxiety, lack of sleep, hot flashes, and, as a result, tension headaches.
These symptoms can act as triggers for migraine attacks, making headaches more frequent and intense during this period. Migraines tend to become less frequent or go into remission after menopause.
During these significant changes, it is important to talk to your doctor to find treatment options that will allow you to manage your symptoms more easily.
Neurological Factors
As observed, migraine disorders fall under the category of neurological conditions. Consequently, certain neurological aspects can influence your susceptibility to migraines.
Particularly, neurological changes that may lead to migraines include:
- Altered blood flow to the brain, or conditions causing the narrowing of blood vessels
- Changes in brain chemistry and pathways
- Incorrect nerve signaling and neurotransmitter imbalances
Conditions that may lead to these changes include:
- Chronic pain, which over time alters how pain signals are processed in the brain
- Deformities in the shape and size of blood vessels in the brain
- Abnormal pressure in the brain
- Diseases such as stroke, brain tumors, and meningitis
- Inflammatory conditions of the brain
- Traumatic brain injury
Developing migraines can also heighten the risk of cognitive disorders, such as early cognitive decline, memory and concentration issues, psychiatric conditions, and dementia.
Cortical Spreading Depression
Cortical spreading depression (CSD) is characterized by a wave of sustained depolarization, or inactivation of neurons, that moves through brain tissues. This can suppress brain activity, leading to changes in neurons and blood vessels in the brain. Although complex, CSD has been linked to conditions such as seizures and brain ischemia. It is also suggested that CSD may be the underlying mechanism of the migraine aura.
Serotonin Imbalance
As previously discussed, serotonin (5-HT) may play a crucial role in the development of migraine disorders. Serotonin is a chemical messenger that facilitates communication between nerve cells in the brain and body.
While serotonin influences functions such as memory, happiness, learning, sexual behavior, hunger, and body temperature, its deficiency is linked to depression, anxiety, and other health disorders. Serotonin also affects pain perception and vasoconstriction (narrowing of blood vessels).
Research highlights serotonin’s involvement in activating the trigeminovascular nociceptive pathway, a pain-signaling pathway in the brain. Activation of this pathway can trigger or intensify pain perception.
The Impact Of Having Specific Lifestyles
Certain lifestyle factors or drastic lifestyle changes can lead to migraine disorders and trigger migraine attacks. Recognizing your triggers can help you manage or prevent migraine attacks by avoiding these triggers or using rescue medications and techniques (e.g., rest, relaxation techniques, biofeedback).
Stress
Stress, while a normal part of life, can be a significant trigger for recurring headaches in individuals with high stress levels or diagnosed migraine disorders. Studies indicate that chronic stress can alter the brain’s state, increasing the excitability of cortical neurons, leading to changes in brain pathways, mood, and behavior, making even minor stressors potential migraine triggers.
Various stress types, such as high-pressure jobs, long commutes, raising children, or financial stress, can lead to headaches. Interestingly, a sudden drop in stress levels can also trigger a migraine.
Dietary Triggers
Certain foods can trigger migraine attacks by causing blood vessels to dilate or constrict, altering blood flow to the brain. Common dietary triggers include:
- Fermented, pickled, salty, or spicy foods
- Cured meats, aged cheeses, and smoked fish
- Yeast extract, chocolate
- Preservatives containing nitrites and nitrates
- Artificial sweeteners, alcohol (especially beer and red wine)
- Monosodium glutamate (MSG), caffeine
- Certain vitamins and herbal supplements
- High-sugar drinks
Skipping meals and drastic blood sugar changes can also trigger headaches. Note that not all foods listed will trigger migraines in every person with migraine.
Excessive Caffeine Consumption
While a daily cup of coffee can be beneficial, consuming over 100 mg of caffeine can trigger migraines. Caffeine affects adenosine, a chemical that controls brain activity and blood vessel dilation. Inhibiting adenosine can increase brain activity and widen blood vessels, contributing to migraines. However, occasional caffeine use can also alleviate migraines.
Dehydration
Chronic dehydration is common among adults and can lead to various health issues, including migraines. Inadequate hydration may cause brain tissues to shrink and pull away from the skull, causing headaches.
Sleep Patterns
Irregular sleep patterns or disturbances, such as insomnia, can lead to frequent migraine attacks. Interruptions during the night can prevent sufficient REM sleep, increasing proteins linked to headaches. Sleep deprivation can also heighten self-reported pain and influence serotonin, potentially leading to migraines. Chronic migraines can further deteriorate sleep quality, creating a cycle.
The Link Between Emotions And Chronic Migraines
A 2020 study indicates that nearly 80% of individuals with migraine disorders experience depression at some point, with a higher likelihood of anxiety and suicidal tendencies. The relationship between emotional health and migraines is complex, influenced by genetic factors and the impact of migraine-related pain, reduced productivity, and anxiety. Addressing underlying emotional factors may help manage migraine intensity and frequency.
The Connection Between Gut Health And Chronic Migraines
To understand how your gut health may cause you to keep getting migraines, it is important to look at the gut-brain axis. This is a bidirectional (two-way) relationship between the gastrointestinal system and the central nervous system (which is composed of the brain and spinal cord).
It has been seen that gastrointestinal disorders such as celiac disease and irritable bowel syndrome may increase the risk of migraines. However, today, the mechanics of this interaction aren’t entirely clear. Hypotheses suggest that the composition of the gut bacteria, as well as inflammation, stress hormones, and nutritional imbalances, may trigger chronic migraine episodes.
Additionally, 95% of the serotonin available to the body is produced in the intestine. As we have seen above, this chemical can significantly influence the brain pathways and reactions that lead to migraines.
Low-Quality Sleep
In the sections above, we’ve looked at how irregular sleeping patterns or sleep deprivation can increase your risk of suffering from frequent migraine attacks. This occurs because functions such as sleep, mood, pain perception, and, consequently, headaches are controlled by common chemical brain messengers and regions in the brain.
What’s more, when you are not getting enough sleep, your pain threshold lowers, thus making you more susceptible to painful stimuli. Because of this, up to 75% of people with chronic migraines also suffer from sleep disorders such as insomnia. To break this vicious cycle, follow some best practices to stabilize your sleep patterns, such as:
- Aim to sleep 7-9 hours per night.
- Go to sleep and wake up at the same time each day.
- Keep your bedroom clear of devices that emit noise or light.
- Avoid blue light-emitting devices before bed, as these can influence the production of melatonin (the hormone responsible for inducing sleep).
- Unwind before bed with relaxation techniques, breathing exercises, or self-care actions such as a warm bath.
- Treat any underlying disorder that may be causing sleep disturbances, such as obstructive sleep apnea.
It is important to notice that sleeping too much can also trigger migraines.
Pinpointing Triggers Of Chronic Migraines
Migraine triggers vary from one person to another, and they can even change throughout your lifetime. However, learning to recognize what’s at the root of your headache episodes can help you in two main ways:
- It can help you avoid triggers, thus making headaches less intense and less frequent.
- It can help you seek contingency treatments after exposure, such as getting enough rest, lowering stress levels, and following rescue therapy.
No two people will have the same migraine triggers. However, six of the most common triggers you should learn to recognize include:
- Stress
- Hormonal changes
- Changes in your sleep patterns
- Lifestyle changes
- Environmental factors
- Physical triggers, such as allergies or dental problems
If you are unsure how to identify your triggers, consider keeping a journal of your migraine attacks. In your journal, you’ll want to record details of your headache, such as premonitory signs (prodrome or aura), intensity, frequency, duration, and relevant aspects, such as how you felt when the attack happened, what you had for dinner, or notable events that happened before your symptoms started. This journal can help you and your healthcare provider find an adequate treatment to manage your migraine attacks.
Traditional Approach To Addressing Persistent Migraines
Often, the causes and triggers of migraine attacks aren’t well understood. Because of this, patients often resort to conservative lines of treatment that aim to make the symptoms of this disorder more manageable. These treatment options may do very little to cure or modify your disease, but they can help you in the short term to manage the most severe symptoms of migraine.
Some, such as mind-body activities, may also help you better deal with triggers such as stress, sleep problems, and lifestyle changes. Below, we’ll look at the most common treatment options prescribed to individuals with migraines.
Medications
One of the most common lines of treatment for migraines is pharmaceuticals. These can either be preventive or rescue medications, depending on whether they are taken to prevent an attack or reduce the intensity of an ongoing headache. Preventive treatments include medications to lower blood pressure, anti-seizure medications, and antidepressants. These work by managing the blood flow to the brain and the chemical reactions involved with pain perception.
Rescue treatments are prescribed during an attack, and they often involve pain medications that temporarily block the pathways in the brain related to pain (triptans). Some medications to treat individual symptoms (such as anti-nausea medications) may also be prescribed.
It is important to keep in mind that these medications should only be used to manage episodic, less frequent headaches.
Non-Invasive Solutions
Non-surgical options are alternative treatments that can help you manage the symptoms of migraine disorders. These treatments can help you better deal with triggers and relieve the intensity of a headache attack. These treatment options include:
- Biofeedback: Biofeedback is a form of therapy that can help you learn to recognize negative patterns and make positive adjustments in your body, such as improving your breathing, relieving muscle tension, and gaining focus.
- Acupuncture: Acupuncture can help ease stress and tension and trigger the release of hormones, such as endorphins, that induce feelings of well-being.
- Massage therapy: Massages can help you relax and ease muscle tension, thus staying safe from everyday triggers such as high stress levels.
- Cognitive-behavioral therapy (CBT): CBT is a type of psychological therapy that can help you identify your triggers and reduce the intensity of a migraine attack. It has been seen to reduce the severity and frequency of headaches in 30-60% of patients with migraines.
Mind-Body Therapies
Certain mind-body therapies have been seen to help reduce stress, relieve tension, increase pain tolerance, and boost self-awareness, which is critical to managing how we react to stress and triggers in everyday life.
Some of these therapies, which work by improving the interaction between the body and the mind, include yoga, tai chi, Pilates, meditation, praying or chanting, and guided imagery. In particular, according to studies, mindfulness-based stress reduction techniques can efficiently improve disability, boost quality of life and self-efficacy, and reduce pain and depression in people with migraines.
How NextPain Care Helps Manage Pain With Recurring Migraines
At NextPain Care, we utilize a 3-level approach to address chronic migraines and other types of pain. We begin with the least invasive techniques and supportive behavioral therapies, such as mindfulness, meditation, diet, and exercise plans, to foster relaxation and improve mental focus and physical health.
If these initial treatments prove insufficient, our team will develop a personalized plan that incorporates additional in-office therapies. These may include techniques such as nerve blocks to interrupt pain signals, or radiofrequency ablation to disable the nerves responsible for transmitting pain.
All our treatment plans are tailored to your individual needs and are physician-led, ensuring comprehensive care. We understand the challenges posed by chronic migraines and are committed to supporting you throughout your healing journey, promoting optimal well-being every step of the way.
Take Control and Prevent Migraine Recurrences
Don't let migraines take over. Start managing them today.