Everyone experiences paresthesia at least once in their lives. Think, for example, of when you’ve been sitting cross-legged for too long and you have the sensation that your limb has “fallen asleep.” Or it can happen while you are asleep, often because your arm or hand has gone numb from being twisted under your head.
This “pins and needles” sensation occurs when certain nerves are pressured and are unable to send signals to the brain relating to movement or sensation. Some forms of paresthesia are temporary and benign – and can be resolved by shifting your body’s position.
However, if this symptom is recurring, chronic, or getting worse over time, you should seek an accurate diagnosis: paresthesia can be a telltale sign of a severe condition affecting your musculoskeletal or nervous system (e.g. sciatica, neuropathy, multiple sclerosis).
In this guide, we’ll look at what paresthesia is and what causes pins and needles sensations. We’ll also help you understand how NextPain Care’s multidisciplinary approach can help you address the pain and discomfort caused by the sensation of pins and needles. Let’s get started.
Recognizing The Prickly Sensation
Pins and needles, medically known as paresthesia, refers to burning or prickling sensations that are commonly felt in the limbs but can spread to any area of the body. The most common cause of paresthesia is sustained pressure on a nerve, which can occur when you lie in a certain position for too long or sit with your legs crooked under your body.
Depending on which nerve is pressured, you may experience pins and needles in various locations such as hands, feet, arms, and legs. If these sensations are caused by temporary pressure on a nerve, changing position will restore the normal function of your limbs in no time. However, in some cases, recurring paresthesia or numbness that spreads from your limbs across the body can indicate a severe underlying condition, including damage to the nerves in the central or peripheral nervous systems.
Other Symptoms Associated With Pins And Needles
Paresthesia usually manifests as pins and needles sensations. However, you may also experience a wide range of symptoms in the affected areas, including the following:
- Burning
- Itching
- “Skin crawling”
- Numbness
- Tingling
- Pain (sometimes described as dull)
Paresthesia typically occurs without warning and can develop within minutes when a nerve is compressed. If it results from a pinched, damaged, or irritated nerve, these sensations can continue spreading over time. When it is a symptom of nerve damage (neuropathy), paresthesia tends to occur first in the fingers and toes, progressing towards the hands, feet, arms, and legs. This happens due to a phenomenon known as “axonal degeneration” or “dying back,” where the nerves furthest from the spinal cord and brain are affected first, to protect more critical nerves that support vital organs.
Possible Underlying Conditions
Although pins and needles sensations may occur without an apparent reason, recurring episodes of paresthesia should not go unaddressed. While this condition is often temporary and can be resolved in a matter of minutes, repeated or worsening occurrences may indicate underlying problems with your peripheral or central nervous systems.
Peripheral Neuropathy
One of the most common causes of paresthesia is peripheral neuropathy, a condition that leads to progressive nerve damage, interfering with the normal transmission of signals from the peripheral nerves to the central nervous system. When this transmission is interrupted, you are likely to experience pain, numbness, and pins and needles. Nearly 90% of people with neuropathy have painful symptoms including tingling, burning, and prickling sensations. Causes of nerve damage can include:
- Diabetes (up to 50% of people with diabetes mellitus report neuropathy in some form)
- Exposure to toxins
- Vitamin deficiencies (especially vitamin B12)
- Lifestyle factors (e.g., aging, alcohol consumption, and smoking)
- Certain medications (e.g., chemotherapy)
- Tumors that press on or damage nerves
- Unknown causes (up to 30% of neuropathy cases are idiopathic)
Nerve Compression
Pins and needles can also result from sustained nerve compression, often due to an awkward body position. This can occur if you fall asleep with your arm under your head or sit in a cross-legged position for a while. Recurring episodes of paresthesia may indicate other compressive factors such as:
- Abnormal tissue growth next to the nerves, such as tumors
- Swelling of tissues around the nerves
- Narrowing of the canal housing the nerves (e.g., peroneal nerve dysfunction, carpal tunnel syndrome, spinal stenosis)
- Bone spurs
- Improper mechanics like poor posture
- An injury causing a body component to press on a nerve
- Medical conditions causing body changes, such as a herniated disc
- Genetic factors, such as having a carpal tunnel that’s too small
An accurate analysis of your symptoms and medical history is necessary to determine the cause of your nerve compression and pinpoint the best treatment for your needs.
Poor Blood Circulation
Poor blood circulation prevents essential oxygen and nutrients from reaching parts of the body, leading to symptoms like pins and needles. Causes can include:
- Lying or sitting awkwardly: Body weight can press on blood vessels, causing limbs to “fall asleep.”
- Atherosclerosis: Plaque buildup in blood vessels like arteries can cause sudden numbness and tingling.
- Blood clots: Can partially or completely block blood flow, causing numbness, pain, and pins and needles, and in severe cases, leading to a heart attack or stroke.
- Diabetes: Uncontrolled blood sugar levels can damage blood vessels, interrupting blood flow.
- Risk factors: Smoking and obesity can affect blood vessel health and lead to poor circulation.
Diabetes, especially if undiagnosed or uncontrolled, can impair blood flow to nerve endings, leading to nerve damage and peripheral neuropathy, conditions commonly associated with paresthesia.
Multiple Sclerosis
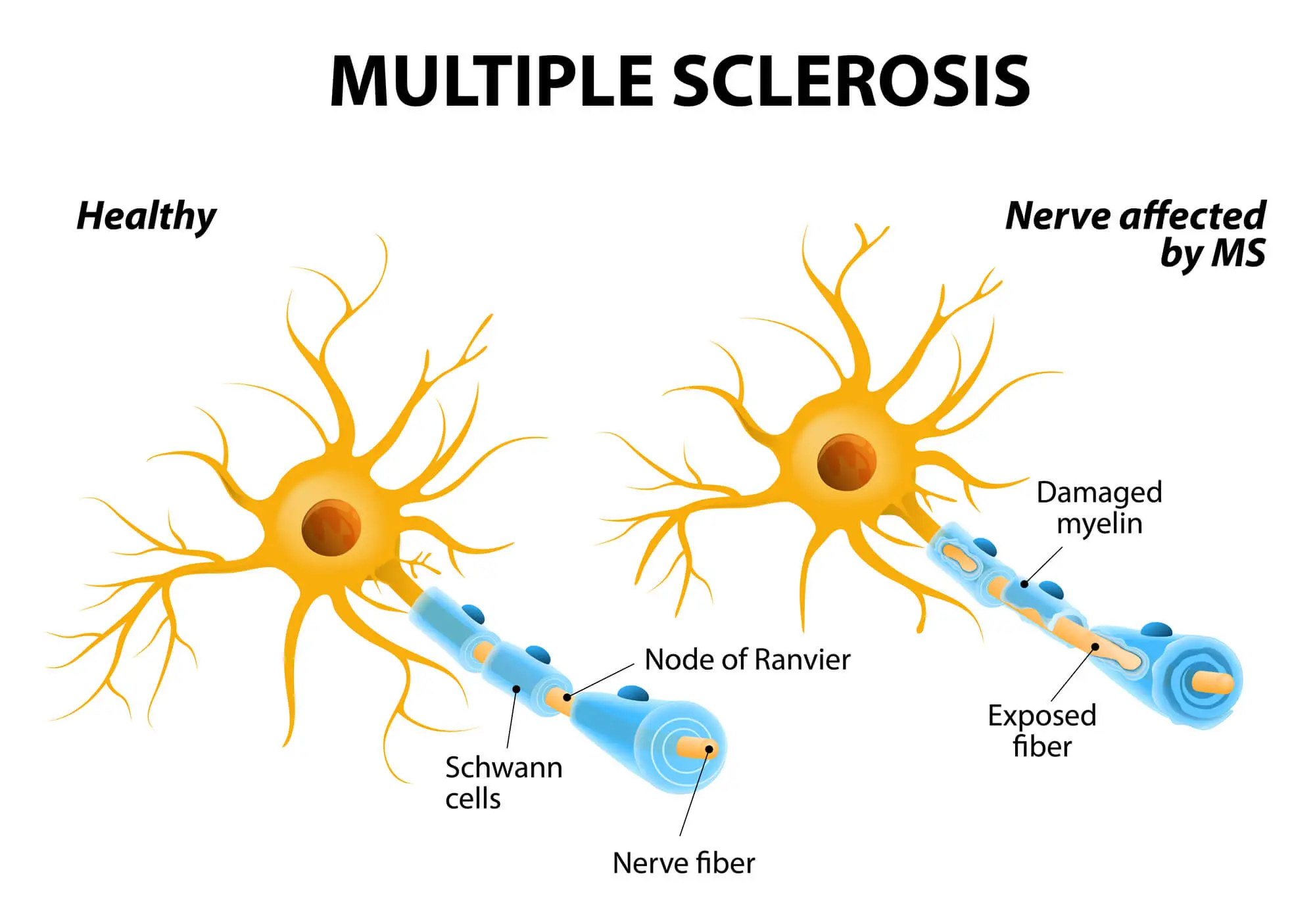
Multiple sclerosis (MS) is a degenerative, lifelong condition affecting the central nervous system. If you have MS, your immune system mistakenly attacks the protective sheath covering nerve fibers, called myelin, disrupting nerve communication and leading to symptoms like paresthesia.
Nerve damage may begin in the hands and feet but tends to progress to other nerves across the body, eventually leading to various degrees of disability. Pins and needles sensations, alongside numbness, tingling, and pain, are some of the early symptoms of multiple sclerosis (MS).
Fibromyalgia
Fibromyalgia is a chronic disorder that causes widespread musculoskeletal pain across the body. The pain caused by fibromyalgia is often described as aching, burning, or throbbing, and it is accompanied by a wide range of symptoms, including paresthesia, mood issues, fatigue, memory problems, and poor sleep quality.
In people with fibromyalgia, painful sensations are amplified due to dysfunction in the way the central nervous system processes painful and non-painful stimuli. It is estimated that today, around four million people in the US – or 2% of the adult population – have fibromyalgia in some form.
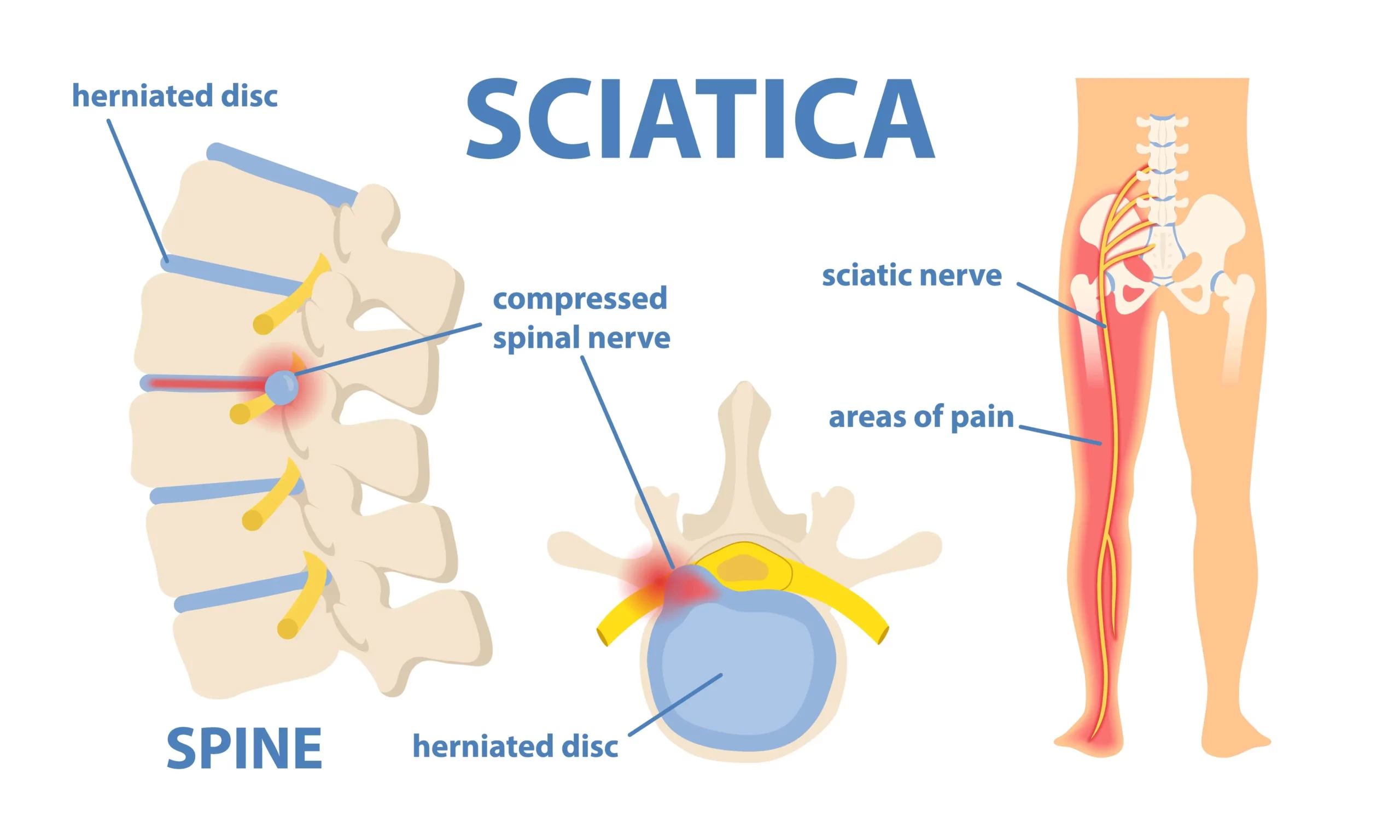
Sciatica
Sciatica is one of the most common reasons for pins and needles sensations, numbness, and tingling, especially those occurring in the buttocks, hips, legs, feet, and toe areas. Sciatica occurs when the sciatic nerve is pinched, irritated, inflamed, or damaged.
There are two sciatic nerves in your body, one on each side, running from the lower back to the feet. These nerves are among the largest and longest in the body, and they are responsible for transmitting signals relating to touch, temperature, pain, vibration, and movement between the brain and the lower part of the body.
There are several conditions that cause a sciatic nerve to become compressed or irritated, including:
- Spinal stenosis
- Old and new injuries (e.g. fractures or dislocations)
- Herniated or bulging discs
- Poor posture
- Inactivity and prolonged sitting
- Weak core and back muscles
- Occupation, especially if it involves repetitive or forceful movements of the spine
- Risk factors such as aging and obesity
- Medical conditions such as diabetes
Around 40% of people will experience at least one episode of sciatica, and this condition tends to resolve on its own within three to twelve weeks.
Nonetheless, if your symptoms are not going away or getting worse, it is important to seek an adequate line of treatment that involves continuous support. This is because sciatica-like pain can conceal more severe underlying diseases, which may derive from systemic inflammation. Tackling this root cause is the first step to regaining your musculoskeletal health.
Raynaud’s Disease
Raynaud’s disease, also called Raynaud’s phenomenon, occurs in around 3-5% of the population. In people with this disorder, the body triggers an abnormal response to cold or stress, causing spasms in small blood vessels located in certain areas of the body (usually the hands and feet). These abnormal spasms (known as vasospasms) reduce blood circulation, which can lead to a range of symptoms, including paresthesia, numbness, tingling sensations, pain, and skin color changes.
How Are Pins And Needles Sensation Connected To Nerves?
To understand why you experience pins and needles in response to dysfunction of the nervous system, it is important to clarify the role that nerves play in carrying sensations. Here’s a simplified overview:
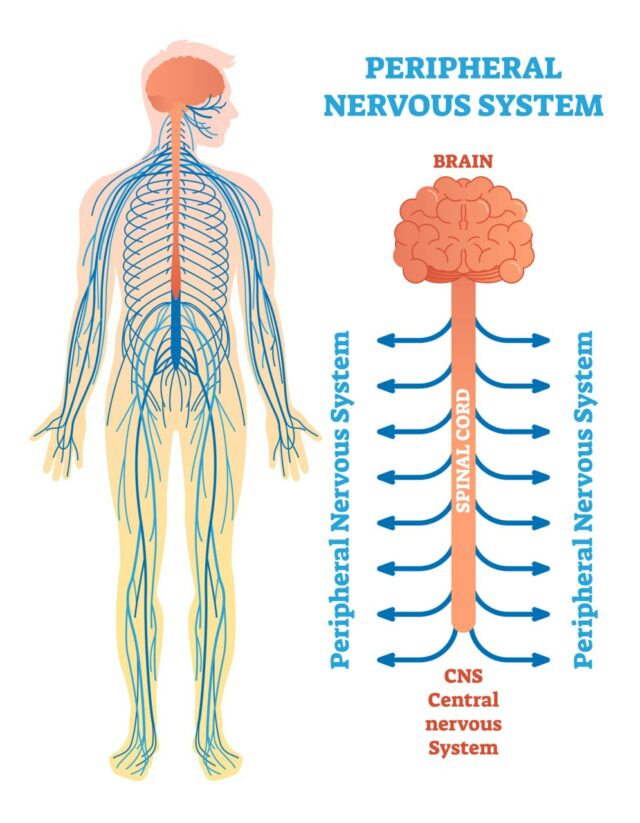
The nervous system is subdivided into two main parts:
- The central nervous system: The nerves located within the brain and spinal cord.
- The peripheral nervous system: The nerves located across the body, outside of the brain and spinal cord.
The nerves in the peripheral nervous system are responsible for carrying signals from different areas of the body to the brain, where they will be processed. These signals can relate to:
- Sensations: These are carried by sensory nerves and involve signals relating to touch, pain, vibration, and temperature.
- Movement: These are carried by motor nerves and include signals relating to muscle movement, coordination, and gland function.
- Autonomic signals: The autonomic nerves regulate functions we don’t have direct control over, such as heartbeat, respiration, digestion, and blood pressure.
When the nerves responsible for carrying motor and sensory signals are compressed, damaged, or inflamed, they work at a suboptimal level, preventing signals from reaching the brain. This translates into a sensation of numbness and an altered response to stimuli, such as being unable to feel temperature and touch.
In severe cases, such as with MS or specific forms of neuropathy, the autonomic nerves can be affected too, causing sexual dysfunction, irregular heartbeat, digestive problems, and loss of bladder or bowel control.
When A Prickly Sensation Is No Longer Normal
Now that you understand why you should not underestimate recurring episodes of numbness and pins and needles sensations, let’s look at when you should seek medical care.
Paresthesia can appear in two forms:
- Temporary: Also known as transient paresthesia, this is the most common form of pins and needles. It is commonly caused by temporary pressure on a nerve, does not last long, and can be resolved by shifting your position.
- Chronic: Chronic paresthesia can last for weeks or months, progress over time, or recur regularly. This is a symptom of an underlying condition that warrants medical attention.
Other signs that should prompt you to see a doctor include:
- The numbness is accompanied by persistent, dull pain.
- Paresthesia is interfering with your daily life.
- You have other symptoms, including reduced range of motion, extreme sensitivity to touch, sleep problems, and disability.
Diagnostic Procedures And Tests
As we have seen above, pins and needles are symptoms associated with more than one condition. Seeking an accurate diagnosis is the first step to finding the best line of treatment for your needs. Your healthcare provider will use a range of diagnostic tools to pinpoint the specific cause of your symptoms. These often include:
- Physical examination: A physical exam, which may include a review of your symptoms and medical history, is needed to determine the extent, location, and intensity of your paresthesia. Your doctor will also use manipulation and palpation to better understand which locations are affected by numbness, pain, and reduced range of motion.
- MRI or CT scans: Magnetic resonance imaging (MRI) and computerized tomography (CT) scans are used to obtain images of the inner aspect of your body. They can identify abnormal tissues or mechanical problems that are compressing a nerve.
- Electromyography: This test assesses the ability of nerves to function properly and the quality of nerve signal transmission. It may help identify nerve or muscle dysfunction.
- Blood tests: Blood tests are prescribed when the suspected cause of your paresthesia is a medical condition such as diabetes.
Your doctor may also take biopsies (samples) of your skin to assess the count and function of nerves in the areas of your body where you have pins and needles.
Conventional Treatment Options
The line of treatment chosen to alleviate your symptoms and restore your musculoskeletal health largely depends on the underlying cause of paresthesia. Below, we’ll look at some of the most commonly prescribed therapies for chronic pins and needles.
Physical Therapy
Physical therapy may help restore physical function, especially when paresthesia derives from conditions like sciatica, weak core or back muscles, and inactivity. If the pins and needles sensations are associated with reduced blood circulation, massage therapy and acupuncture may also help support circulation and relieve muscle tension, thus improving nerve function.
Physical therapy is more efficient when combined with necessary lifestyle changes, such as increased activity levels, and therapies that address the systemic inflammation at the root of conditions like diabetes, sciatica, and nerve damage.
Medications
Certain medications may help relieve the symptoms of a compressed or damaged nerve. These include:
- Nonsteroidal anti-inflammatory medications (NSAIDs)
- Painkillers
- Corticosteroid injections
- Capsaicin cream (Capsaicin is the active component in chili peppers.)
- Rubs, balms, and gels that can be applied topically
Specific pharmaceutical therapies may also be recommended to address the underlying condition that is causing your paresthesia. For example, if you have diabetes, you may be prescribed insulin and oral medications to manage your blood sugar levels.
Surgery
Surgical interventions are prescribed when paresthesia begins to interfere with your daily life, cause disability, or do not respond to conservative treatments. Depending on the cause of your symptoms, surgery may be used to:
- Enlarge the passageway that houses nerves to decompress them, such as in the case of carpal tunnel surgery
- Remove tissues that are pressing on the nerve, such as in the case of discectomy when sciatica is caused by a herniated disc
- Correct mechanical issues, such as those deriving from a new or old injury
While surgery is an option, we believe in exhausting conservative measures first.
How NextPain Care Manages Discomfort Caused By Tingling Sensations
The sensation of pins and needles can be a frustrating and disruptive experience, affecting your ability to carry out daily activities. We understand how challenging this can be and are here to help. At NextPain Care, we focus on providing compassionate, evidence-based treatments to manage your symptoms and improve your quality of life.
We begin by getting to know your condition thoroughly to understand what’s causing your symptoms. Our first step is to try non-invasive treatments. This means making simple lifestyle changes like adjusting your workspace and adding specific exercises to help your nerves function better. Physical therapy plays a big role in reducing discomfort and improving your movement. We also offer support for managing any stress or anxiety that might make your symptoms worse, and we might suggest supplements to boost your nerve health.
If these initial steps don’t provide enough relief, we move to the next level of care. This might involve medications like NSAIDs, neuropathic drugs, or muscle relaxants to help ease your discomfort. We also offer treatments like nerve blocks or localized injections for more targeted relief. For more persistent or severe cases, we have advanced, minimally invasive procedures such as nerve stimulation.
Our multidisciplinary team collaborates to create personalized treatment plans, combining their expertise to address all aspects of your condition comprehensively. This integrated approach ensures you receive holistic care aimed at improving your overall health and well-being.
We Manage Prickly Sensations Related To Nerve Discomfort
Chronic inflammation is known to be one of the most impactful causes of several chronic diseases affecting the population today, from diabetes to cardiovascular disorders, arthritis, and allergies. The customizable approach developed by NextPain Care aims to tackle pain caused by inflammation. By focusing on your specific needs and offering continuous support, we aim to alleviate your symptoms and enhance your quality of life. We can help ease a range of symptoms and conditions, including those listed below.

Peripheral Neuropathy Treatment
Peripheral neuropathy is a condition that can cause severe pain, impacting daily life. At NextPain Care, we use evidence-based practices to provide relief from the painful symptoms of peripheral neuropathy, adhering to the highest standards set by medical...

Fibromyalgia Treatment
Fibromyalgia is a chronic condition characterized by widespread pain, fatigue, and other challenging symptoms such as tender points and sleep disturbances. At NextPain Care, we use evidence-based approaches to help manage the painful symptoms of...
Experience The Difference With Specialized Care
At NextPain Care, we prioritize creating a compassionate and supportive environment. We understand that living with the sensation of pins and needles can be tough, but we are here to support you.
Together, we can work to reduce your discomfort, enhance nerve function, and help you enjoy life more fully. Our commitment is to provide you with the best possible care; ensuring your comfort and recovery are always our top priorities.
Concerned about the prickly sensation you're feeling? Let NextPain Care help you uncover the cause and find effective treatment.