In our everyday lives, we perform movements such as walking, jogging, climbing stairs, or bending down to tie our shoes almost automatically. If we can perform these movements, it is thanks to the knees’ complex structure of bones, ligaments, tendons, cartilage, and muscles, which gives them exceptional mobility.
However, it is often too easy to take such a range of motion for granted. Over time, injuries, diseases, and health conditions can significantly reduce your knees’ range of motion and have a profound impact on your ability to remain functional in your daily life.
Fortunately, with the three-level care system at NextPain Care, we provide you with step-by-step options for treatments that can help you improve your knee mobility.
How Does Reduced Knee Range Of Motion Affect You?
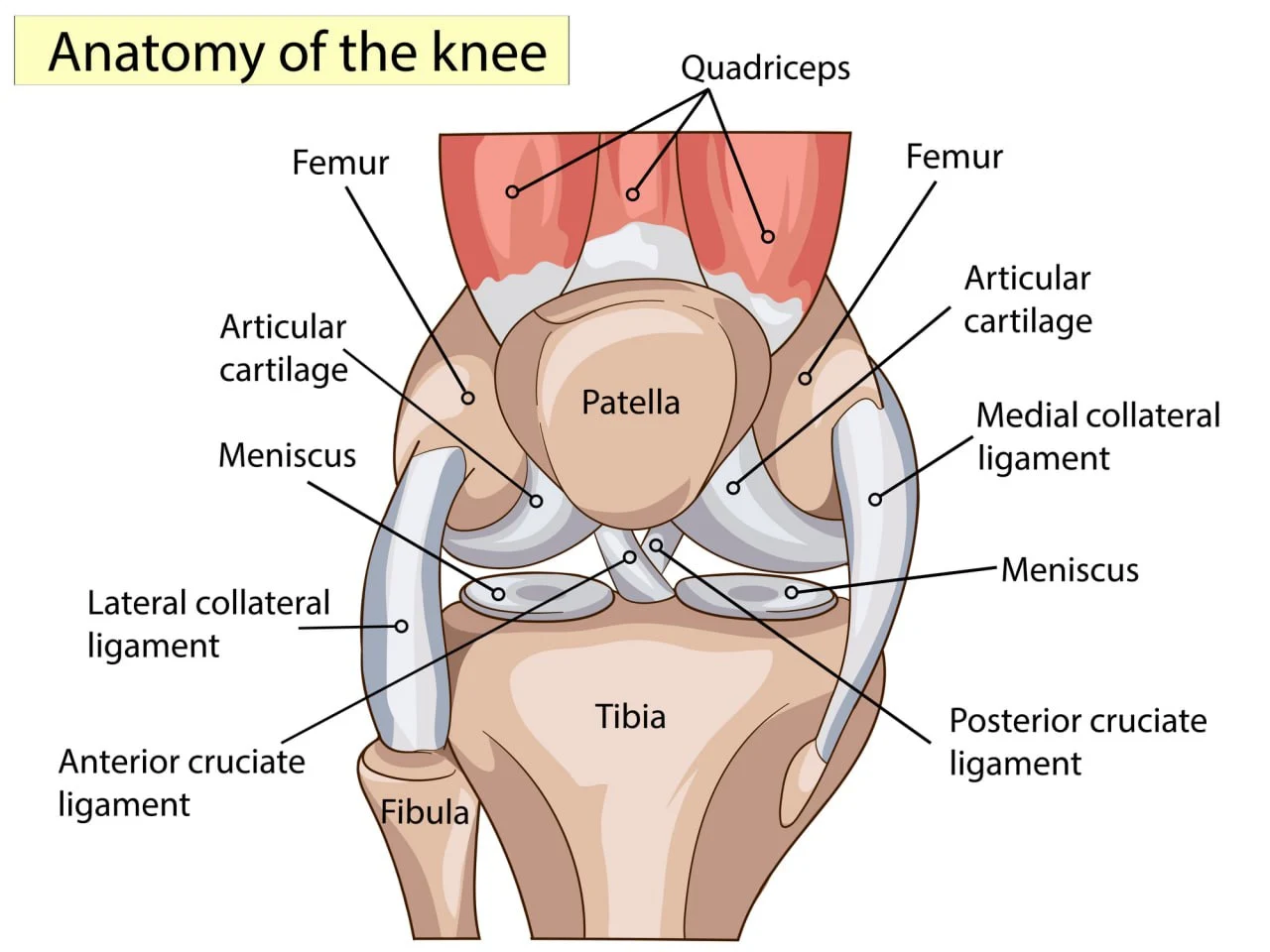
The knee plays a vital role in bearing and redistributing loads during walking or running, absorbing shock, and balancing the body as it moves through space. This complex joint links the upper leg bone (the femur or thigh bone) and the lower leg bones (fibula and tibia, or shin bone), which are protected by a frontal flat bone called the patella.
These bones are connected by four ligaments:
- Anterior cruciate ligament (ACL)
- Posterior cruciate ligament (PCL)
- Medial collateral ligament (MCL)
- Lateral collateral ligament (LCL)
Each bone is also connected to the muscles of the upper and lower leg by tendons. The knee joint is kept lubricated and protected from friction damage by cartilaginous tissues, which act as shock-absorbing “cushions.”
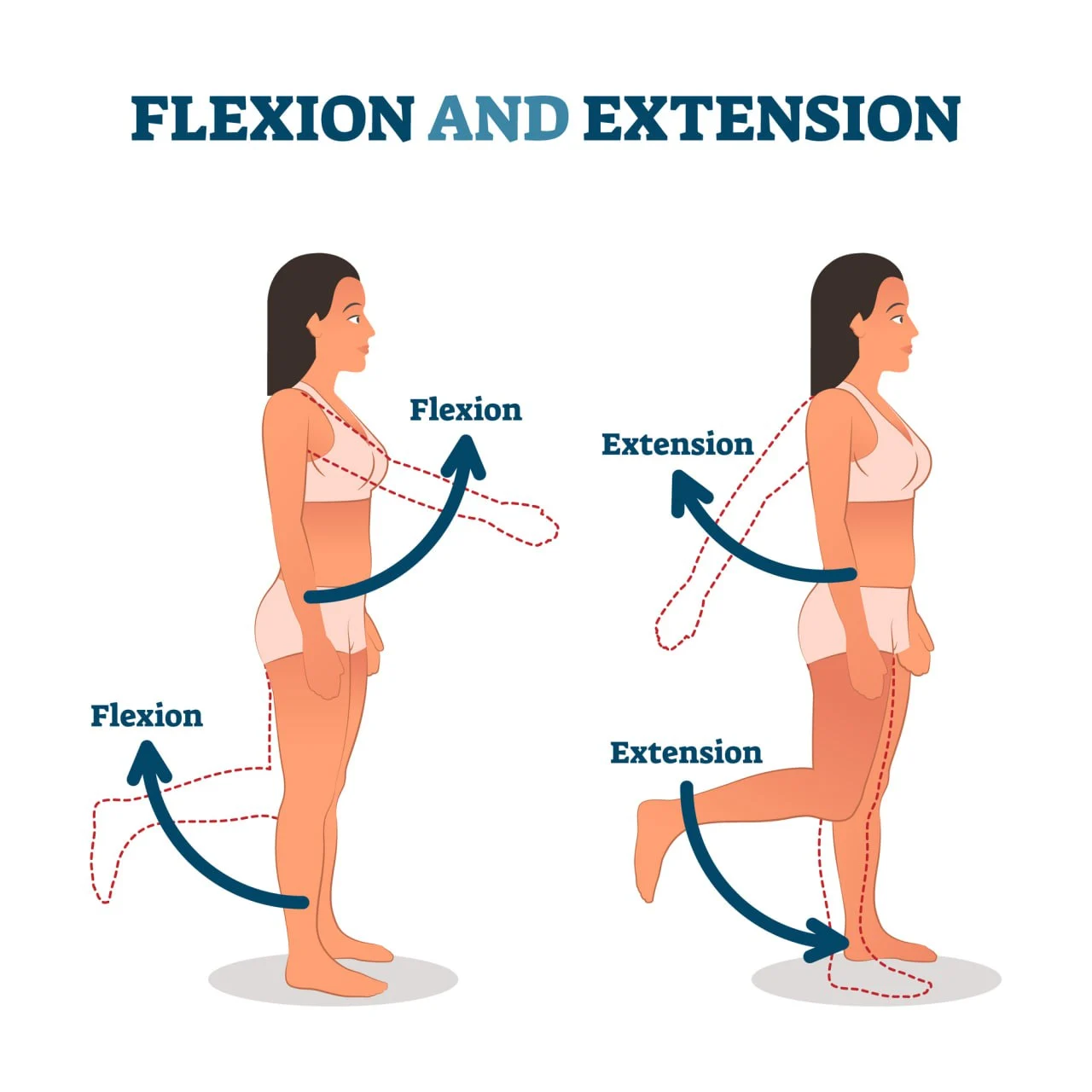
This complex structure enables the three main movements of the knee:
- Extension (straightening the knee)
- Flexion (bending the knee)
- Lateral rotation
The full range of motion (ROM) of the knee refers to its complete movement potential. Limited ROM describes a condition where the knee joint is unable to move through its full range of motion.
Limited ROM may occur due to infection, injury, mechanical issues, inflammation, and degenerative diseases like osteoarthritis. It is estimated that up to a quarter of the population may experience a reduced range of motion to some extent.
A slight or short-term reduction in knee ROM may be due to poor muscle conditioning or minor injuries. These are temporary conditions that can be addressed easily or resolved by themselves with at-home care.
However, in some cases, the inability to move the knee through its full ROM is a symptom of an underlying condition, such as arthritis, that requires immediate medical attention.
When left unaddressed, limited ROM can have significant consequences, including:
- Limiting your ability to remain functional and active in your daily life
- Pain, stiffness, and further loss of range of motion
- Significant impairment and disability
- Preventing you from living independently or aging in place
- Leading to imbalances, mechanical issues, and poor posture, particularly if present in only one knee
- Relative disuse of one knee, and subsequent loss of muscle strength
For athletes and sportspeople, limited range of motion may also impact the outcome of resistance training, leading to decreased performance.
Conditions Associated With Limited Knee Mobility
As we get older, the components of the knee may suffer progressive degeneration, which translates into a normal, age-related loss of range of motion. However, some conditions can impact your knee health and reduce your knee mobility drastically.
Below, we’ll look at the health events and diseases that may compromise your knee’s ability to move as it should.
Chronic Knee Pain
Chronic knee pain often arises from degenerative conditions, traumatic injuries, overuse, or mechanical issues. If left unaddressed, chronic knee pain can lead to knee disuse, muscle atrophy, and disability.
It is estimated that one in four adults suffers from long-term knee pain, and this prevalence is on the rise due to the aging of the population and increasing rates of obesity.
Chronic knee pain is often characterized by an excessive and sustained inflammatory response. In turn, high levels of inflammation can lead to swelling, pain, and stiffness, which can restrict joint movement and prevent the knee from flexing or extending to its full range of motion.
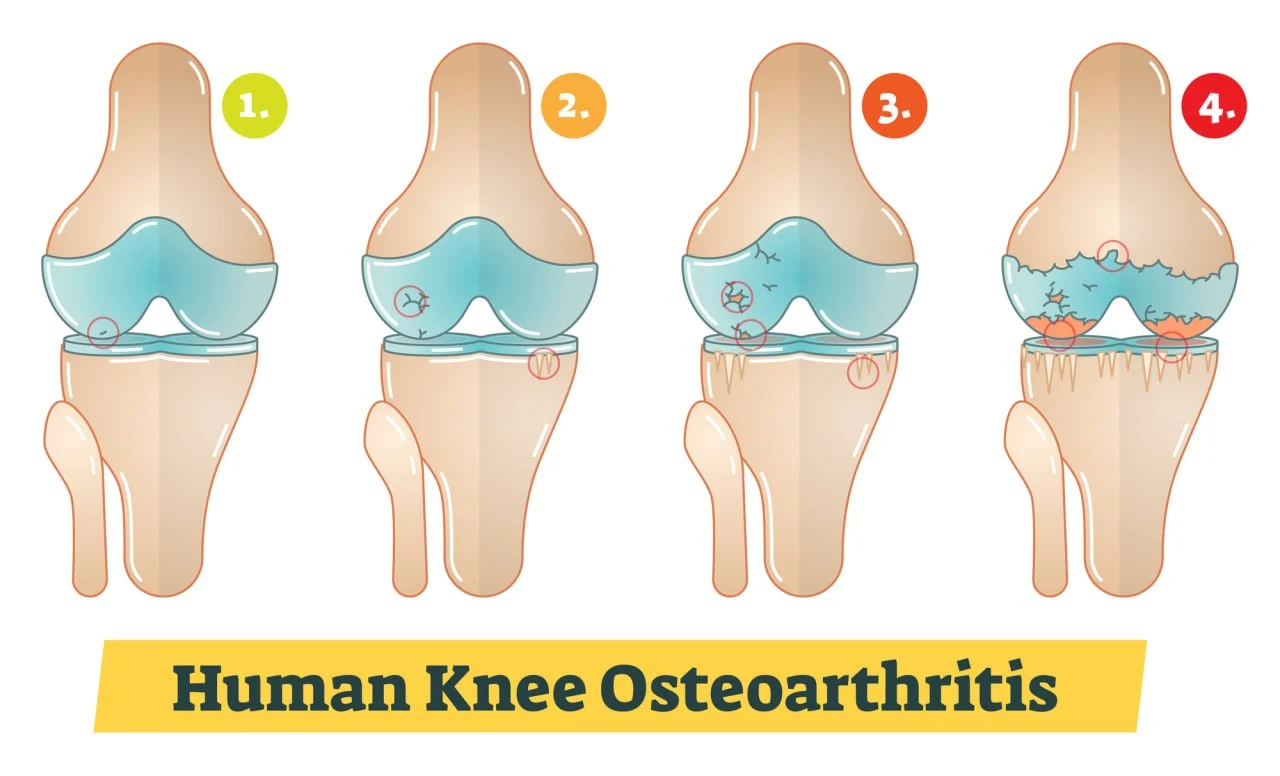
Osteoarthritis
Osteoarthritis (OA) is an inflammatory condition of the joints that leads to the progressive degeneration of the cartilage. As the cartilage breaks down, the joint’s components are exposed to friction and shock damage during movement, leading to damage to bones, ligaments, and tendons.
Over time, osteoarthritis can cause the formation of abnormal bone growths (bone spurs) and deformities, which prevent the knee from moving as it normally should.
Often caused by natural age-related wear-and-tear, overuse, and poor mechanics, osteoarthritis (OA) is the most common form of arthritis and the leading cause of disability in the elderly. That’s because, if left unaddressed, osteoarthritis can compromise the mechanics of the knee joint and cause irreversible damage to the components responsible for safeguarding its full range of motion.
Like other forms of arthritis, OA also causes joint pain, stiffness, swelling, clicking noises, and “catching” sensations, which can make knee movements even more undesirable.
Injuries And Tissue Damage
Traumatic injuries that cause damage to tissues like bones, ligaments, and tendons can have a long-lasting impact on the knee’s ROM. This can occur for multiple reasons:
- An acute knee injury can permanently compromise one or more of the components of the knee.
- Lack of rehabilitation after an injury or surgical procedure can cause long-lasting damage.
- Injury and immobilization can lead to relative disuse of the knee, which translates into a subsequent loss of muscle mass and strength.
- Abnormal scar tissue can build up after a fracture or surgical intervention (e.g., after an anterior cruciate ligament reconstruction), binding components of the knee together and limiting their mobility. This condition is known as arthrofibrosis.
- Unsuccessful surgical interventions or inadequate recovery from a broken bone can impact normal knee mechanics and expose the joint components to excessive stress.
Some injuries that can lead to a loss of ROM include dislocations and fractures, as well as torn ligaments, tendons, and cartilage.
Infections
Some infections caused by bacteria, viruses, and fungi tend to target the joint’s structures. For example, in children, hip infections can lead to pain, swelling, and subsequent ROM issues.
In the knee, the most common infection is septic or viral arthritis. This condition occurs when germs and viruses travel through the bloodstream from other infected areas of the body (e.g., following an animal bite or penetrating injury). Some of the viruses that may cause septic arthritis include hepatitis B, hepatitis C, and the Zika virus.
Septic arthritis causes symptoms like swelling, pain, and stiffness, which translate into difficulty moving the joint and a reduced range of motion. Around 20,000 cases of septic arthritis are reported in the US alone each year.
Muscle Weakness
The muscles of the upper and lower leg play a vital role in initiating and controlling knee movements. When these muscles lose mass, strength, or flexibility, you may struggle to bend or extend the knee fully.
Some muscle conditions associated with reduced ROM include:
- Muscle tightness. Tight muscles can impact the flexibility of the knee, preventing it from stretching or flexing as it should.
- Muscle weakness. Without enough muscle power, you may be unable to extend or bend your knee, as well as keep it bent or extended.
- Muscle atrophy. A severe loss of muscle mass that occurs after periods of immobilization or disuse can significantly compromise knee mobility.
Poor muscle conditioning can create a vicious cycle that can further restrict your ROM: weak muscles may not support daily movements like climbing stairs, walking, or jogging, which, in turn, can lead to a further loss of strength and mobility.
Neurological/Neuromuscular Conditions
Some neurological and neuromuscular conditions interfere with the normal transmission and processing of nerve signals relating to muscle movements. When these signals are unable to reach the brain or are not properly processed, you may become unable to control muscle movements.
Disorders that cause damage to muscles, the brain, or the nerves in the central and peripheral nervous system include:
- Cerebral palsy
- Spinal cord injury
- Multiple sclerosis
- Stroke
- Brain or head injury
- Muscle dystrophy
- Contracture deformities (conditions that cause components of the joint to become permanently fixed)
Without adequate care, these conditions can lead to severe complications, including muscle atrophy, numbness, and disability.
When To Seek Professional Medical Help
If you have experienced a minor trauma such as a knee ligament sprain, your loss of ROM will likely be a temporary condition, mostly associated with the body’s inflammatory response to injury. In this case, at-home care will be enough to ease pain and swelling and help you regain your knee function in two to four weeks.
However, if you suffer from a degenerative joint condition or chronic pain, the loss of range of movement can be recurring, long-lasting, and incredibly impactful on your day-to-day life. Additionally, reduced knee mobility may be a symptom of an underlying neurological disease, which requires immediate medical attention.
Generally, you should see your doctor if:
- You can’t fully straighten or bend one or both knees
- You frequently suffer from reduced knee mobility or recurring ROM problems
- Your daily activities are affected by the loss of ROM
It is important to note that, as you age, you are likely to lose joint mobility to some extent.
Although this is normal, you should be able to retain what’s known as a “functional range of movement.” This is the minimum range of movement your knee needs to allow for everyday activities, like climbing stairs, bending, walking, sitting down, standing up from sitting, riding a bike, squatting, and tying your shoelaces.
A healthy knee’s full range of motion is 135 degrees. Most daily activities require full extension but only 110-120 degrees of knee flexion. In turn, losing a few degrees of knee flexion won’t affect your daily activities, while not being able to fully extend your knee can significantly impact your mobility.
Measuring And Diagnosing Limited Range Of Motion
To understand how a limited ROM is diagnosed and measured, it is firstly important to clarify the difference between active, passive, and active assisted range of motion. Let’s look at these different ways of measuring ROM below:
Active ROM: Active range of motion refers to how much you can flex and extend the knee autonomously. When assessing active ROM, you’ll be bending and extending your knee by contracting your muscles, without external help.
Passive ROM: Passive ROM is the measure of how much your knee can flex and extend when someone moves or stretches your leg. A physician or specialized machine will help you bend and extend your knee if you are unable to do so by contracting your muscles.
Active assisted ROM: Active assisted ROM measures how much you can move your knee with some assistance.
Although it is normal for passive knee ROM to be greater than active ROM, these two measures should be similar in a healthy, pain-free knee.
According to a study conducted by the Centers for Disease Control and Prevention (CDC) on the range of motion of different joints, a healthy knee should be able to move as follows:
| Age 20–44 | Age 45–69 | |||
| Motion | Females | Males | Females | Males |
| Knee Flexion | 141.9° | 137.7° | 137.8° | 132.9° |
| Knee Extension | 1.6° | 1.0° | 1.2 ° | 0.5° |
The knee should also be able to rotate internally by 10 degrees and externally by 30-40 degrees. Normal passive knee flexion can be as much as 150°, while passive knee extension can be up to 10° of hyperextension.
Given these values, your doctor will determine the extent of your loss of ROM and diagnose any underlying condition that may be limiting your knee mobility.
Some of the diagnostic tools and techniques used in the process include:
Medical exam: Your doctor will carry out a physical examination, a review of your symptoms, and assessments of your medical history.
Imaging tests: Imaging tests like X-rays may be used to obtain a clear picture of the inside of your knee and to determine the presence of abnormal tissue (e.g., tumors) and mechanical issues.
Goniometry assessment: Using a goniometer is the most accurate way to diagnose the extent of ROM loss. A goniometer is an instrument designed to measure angles. It is composed of a central round body representing 360 degrees of motion and two arms, one stationary and one moveable.
To measure your range of knee flexion and extension, your doctor will carry out the following steps:
- You will be asked to lie on your back on a flat surface and straighten your leg.
- The goniometer will be positioned so that the central body of the instrument is against the side of the knee, on the lateral femoral epicondyle (the outer part of the knee).
- Keeping the goniometer in place, your physician will set the stationary arm along the outer thigh, in line with the greater trochanter (the bony lump located at the top of the thigh).
- The moveable arm of the goniometer will be set along the lower leg, in line with the lateral malleolus of the ankle (the bony lump visible on the outer part of the ankle).
- The physician will ask you to use your muscles to straighten the leg and measure the knee extension.
- To measure knee flexion, your doctor will ask you to bend your knee as far as you can by bringing your foot closer to your buttocks.
Self-assessment: You can estimate your knee flexion and extension without a goniometer. To do so, follow these steps:
- Lie on your back on a firm, flat surface.
- Straighten the leg using your muscles and try to slide your hand underneath the knee.
- If you can’t fit any of your fingers, your knee is hyperextended.
- If you can slide all of your fingers under the knee, you are lacking approximately 5 degrees in extension.
- To estimate knee flexion, slide your foot along the surface towards your buttocks. Then, measure the distance between your buttocks and your heel. This method can be used to check your progress and try to improve knee flexion, but it won’t give you a precise measurement.
Other methods: To obtain a more accurate measurement of your knee ROM at home, you can download a goniometer app. You may also ask a friend or family member to help you measure your knee extension and flexion.
Conventional Treatment Options
As seen above, treating a temporary reduction in ROM is a matter of finding the right at-home remedies, such as rest, icing, and compression. However, if your mobility issue is long-lasting or recurring, your first step should be obtaining an accurate diagnosis.
Once you and your physician have an understanding of what’s affecting your knee, you may be recommended one or more of the following treatments:
Compresses: Icing a new injury such as a sprain can reduce swelling and stiffness by preventing the build-up of fluids around the injured tissues.
In the case of old injuries that still cause pain, chronic pain conditions, or inflammatory diseases like arthritis, hot compresses can support the circulation of blood and nutrients and relax tense muscles.
Ultimately, compresses can ease painful flare-ups, which may otherwise get in the way of your knee mobility.
Exercise: If the loss of ROM is caused by muscle weakness or tightness, you may benefit from physical therapy and exercise. A therapist will guide you in the process of exercising your knee, avoiding further injuries, improving flexibility, and rehabilitating weak muscles.
Shockwave therapy: Extracorporeal shockwave therapy (ESWT) is a form of treatment that uses acoustic waves delivered through the skin. The low-frequency waves support the healing of damaged tissues, promote circulation, and stimulate nerves at the site of injury.
According to a 2020 study, this therapy can help improve ROM in people with knee osteoarthritis.
Surgery: Diseases such as arthritis and traumatic injuries may severely compromise the components of the knee. Surgical interventions like knee arthroplasty may be used to replace these worn-out components with an artificial joint.
Given the lengthy rehabilitation times and risks involved with this type of invasive intervention, surgery is only recommended when other treatments have failed.
Fortunately, there are other treatment options for limited ROM. Below, we’ll explore how the approach pioneered by NextPain Care can help you restore your knee function.
The NextPain Care Approach For Limited Knee Motion
If you’ve lost mobility in your knee, it can impact every aspect of your life. You might struggle with everyday tasks like climbing stairs, tying your shoelaces, or enjoying your favorite sports. Addressing this issue is crucial for restoring knee function and improving your quality of life.
As a physician-led company, NextPain Care integrates physical therapy and behavioral therapy within our innovative three-tier system. Our approach is grounded in evidence-based outcomes and data, ensuring that our treatments are both effective and scientifically validated.
We start with conservative treatments such as physical therapy, lifestyle modifications, and medication management to manage pain effectively and non-invasively. When these minimally invasive treatments are insufficient, we turn to advanced options like epidural steroid injections, nerve blocks, and spinal cord stimulation for more comprehensive pain relief.
This unique blend allows us to provide holistic care that helps you to live a fuller, pain-free life.
Reclaim Knee Movement and Comfort
A loss of ROM in the knee can be a profoundly impactful condition, but it should not be seen as a normal part of life.
Whether you’re dealing with chronic pain or an underlying condition like osteoarthritis, the NextPain Care methodology offers a way to improve your knee mobility with minimal invasiveness.
Focus on your knee health by choosing NextPain Care as your partner in managing reduced mobility. Let us help you take the first steps towards better knee function.
Regaining limited mobility and range of motion in the knee is possible.