Mild cramps and minor discomfort are a normal part of certain phases of the menstrual cycle. However, up to a third of women of reproductive age experience excruciatingly painful periods, accompanied by intense menstrual cramps that start days before menstruation and continue long after their periods end. These painful sensations aren’t just debilitating – they can also be life-limiting, interfering with daily life and affecting your ability to work or engage in social activities.
Painful periods – a condition known as dysmenorrhea – are not normal and can be a symptom of a more serious underlying condition. With an accurate diagnosis provided by the specialists at NextPain Care and an extensive care plan, you can identify and address the root causes of your condition without medications or surgery. Learn more below.
How Do Menstrual Periods Cause Pain?
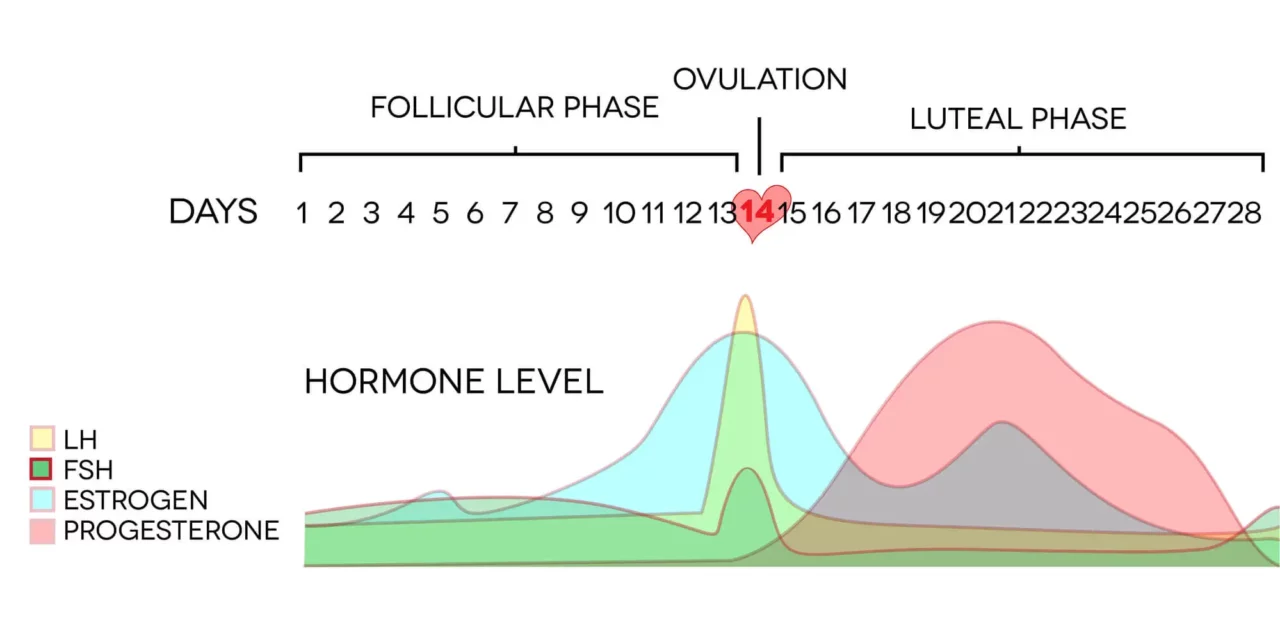
The menstrual cycle is a complex process involving several glands, hormones, and organs. It consists of four main phases:
- Follicular: During the follicular phase, which starts on the first day of your cycle and lasts for up to 14 days, the body releases hormones that stimulate the production of follicles on the internal surface of an ovary. Only one of these follicles will then mature into an egg.
- Ovulation: During ovulation, a mature egg transfers from the ovary to the uterus via the Fallopian tube. Ovulation may last between 16 and 32 hours and represents the time when a woman is most fertile.
- Luteal: After ovulation, the interior lining of the uterus (endometrium) begins to grow, thicken, and swell in preparation for pregnancy. If you are pregnant, the endometrium will support the growth of the fetus and safeguard the egg from microbial invasions.
- Menstruation: If the egg is not fertilized and you are not pregnant, the body expels the unneeded endometrium through menstruation.
During the menstruation phase, the body produces high levels of a hormone called prostaglandin, which triggers the muscle contractions needed to expel the lining of the uterus. However, these contractions can cause pain, and high levels of prostaglandin may increase inflammation in the uterus and surrounding organs.
Painful menstrual cramps may also be accompanied by other symptoms like constipation, diarrhea, and nausea.
Types Of Period Pain
There are two types of dysmenorrhea:
- Primary dysmenorrhea: If you have primary dysmenorrhea, painful menstrual cramps are the condition itself. They are not caused by another underlying disorder, start just after your menarche (first menstruation), and accompany every menstrual cycle you experience. The pain from primary dysmenorrhea can range from mild to severe, change over time, and disappear after two or three years. This is the most common form of dysmenorrhea.
- Secondary dysmenorrhea: Secondary dysmenorrhea refers to painful periods caused by another underlying medical condition. This type of dysmenorrhea is usually more intense and lasts longer than normal menstrual cramps, and it can develop at any point in a woman’s reproductive life. Secondary dysmenorrhea accounts for less than 8% of cases of painful menstrual cramps and is most commonly caused by endometriosis.
Pain Thresholds During Menstruation
Several studies have been conducted to determine how the pain threshold changes across the different phases of the menstrual cycle.
Research published in 2003 showed that pain sensitivity levels were significantly higher in the menstrual and premenstrual phases of the cycle, also due to the rise in prostaglandin. Those who experienced intense pain were also more likely to have a passive coping style and catastrophizing thoughts. On the other hand, studies have shown that the highest pain tolerance occurred during the follicular phase.
Additionally, given that sex hormones such as estrogen influence how the brain processes pain signals, the hormonal fluctuations that occur during the menstrual cycle may worsen the painful sensations deriving from other conditions, including migraine.
Conditions Associated With Extremely Painful Periods
If you have recently developed extremely painful periods, you may have secondary dysmenorrhea. This means that simply treating the pain, cramping, and discomfort you experience during the menstrual cycle isn’t enough to regain your pelvic health. Even worse, when left unaddressed, certain conditions that cause painful menstrual cramps can lead to infertility.
Identifying the root cause of your painful periods is the first step to obtaining an accurate diagnosis and selecting an efficient line of treatment. Let’s look at the most common causes of dysmenorrhea below.
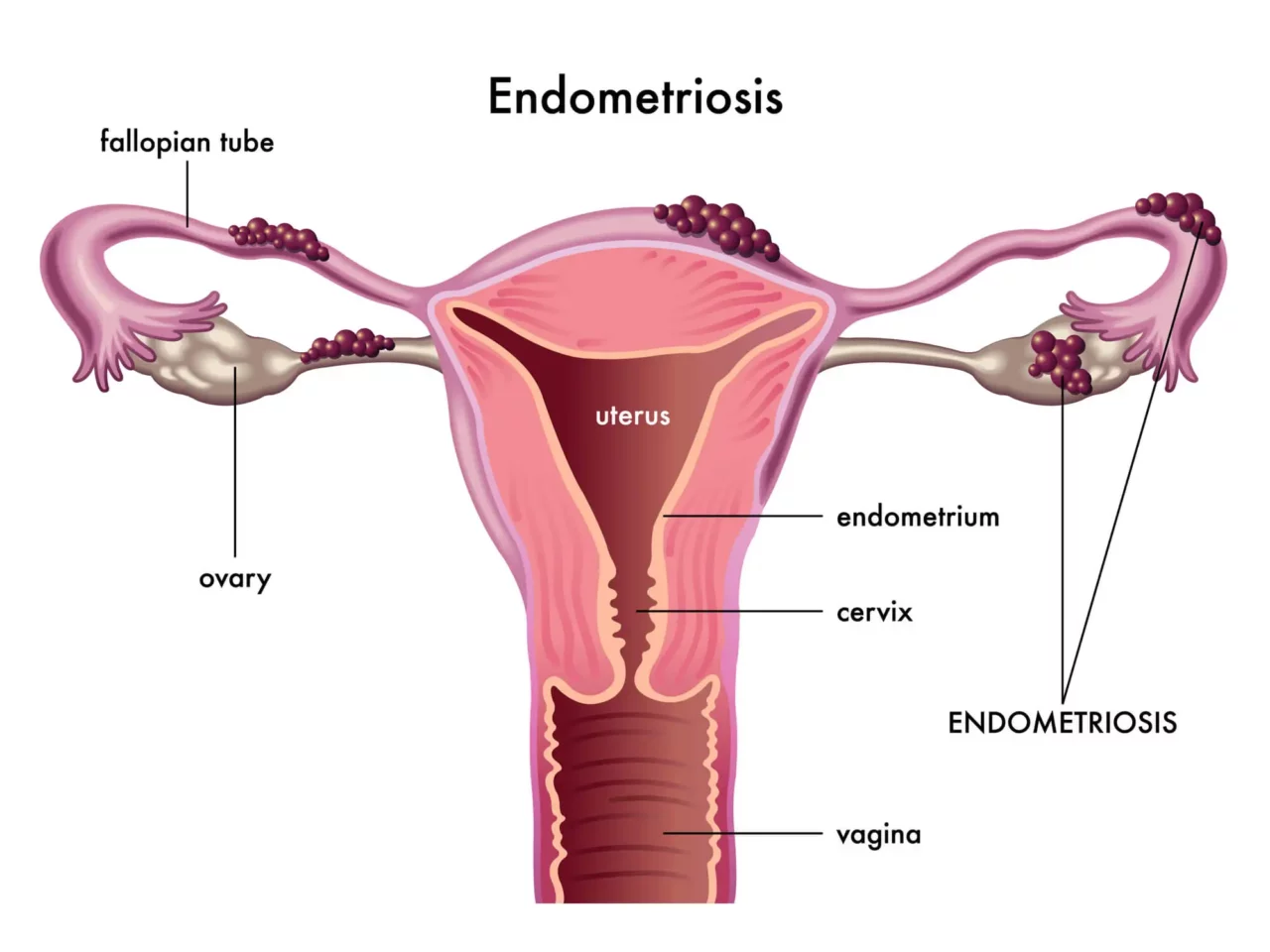
Endometriosis
Endometriosis occurs when endometrial growths (lining of the uterus) that thicken and swell during the luteal phase begin to grow outside the uterus, usually on the ovaries, fallopian tubes, pelvic cavity, cervix, vagina, and bladder.
During the different phases of the cycle, this abnormal endometrial tissue behaves just like the endometrium inside the uterus: it is hormone-dependent and grows and thickens during the luteal phase. However, unlike the endometrium, the endometrial implants outside the uterus are unable to leave the body during menstruation.
This leads to an accumulation of endometrial tissue outside the uterus that continues to proliferate, swell, and thicken with each menstrual cycle. Over time, this inflamed tissue can lead to scarring, cysts, adhesions (binding between reproductive organs), and infertility.
Endometriosis is the most common cause of secondary dysmenorrhea. This condition affects over 6.5 million women in the US alone and causes patients to lose an average of six hours a week of productivity.
Endometriosis is also associated with other life-limiting symptoms, including dyspareunia (pain with sexual intercourse), painful bowel movements, excessive bleeding, and gastrointestinal issues. Despite how common and debilitating endometriosis is, 90% of people with this condition report feeling dismissed or disbelieved by their doctors or loved ones.
Premenstrual Syndrome (PMS)
Around 90% of women of reproductive age experience premenstrual syndrome to some extent. This condition is characterized by a range of symptoms, including emotional tension, anxiety, depressed mood, changes in appetite, poor concentration, and changes in libido. PMS also causes joint or muscle pain, headaches, bloating, acne flare-ups, fluid retention, and constipation or diarrhea.
PMS usually occurs one or two weeks before menstruation begins, and the symptoms ease down when your period starts. Although the causes of premenstrual syndrome are not always clear, it is believed that it may arise due to hormone fluctuations and changes in brain chemicals.
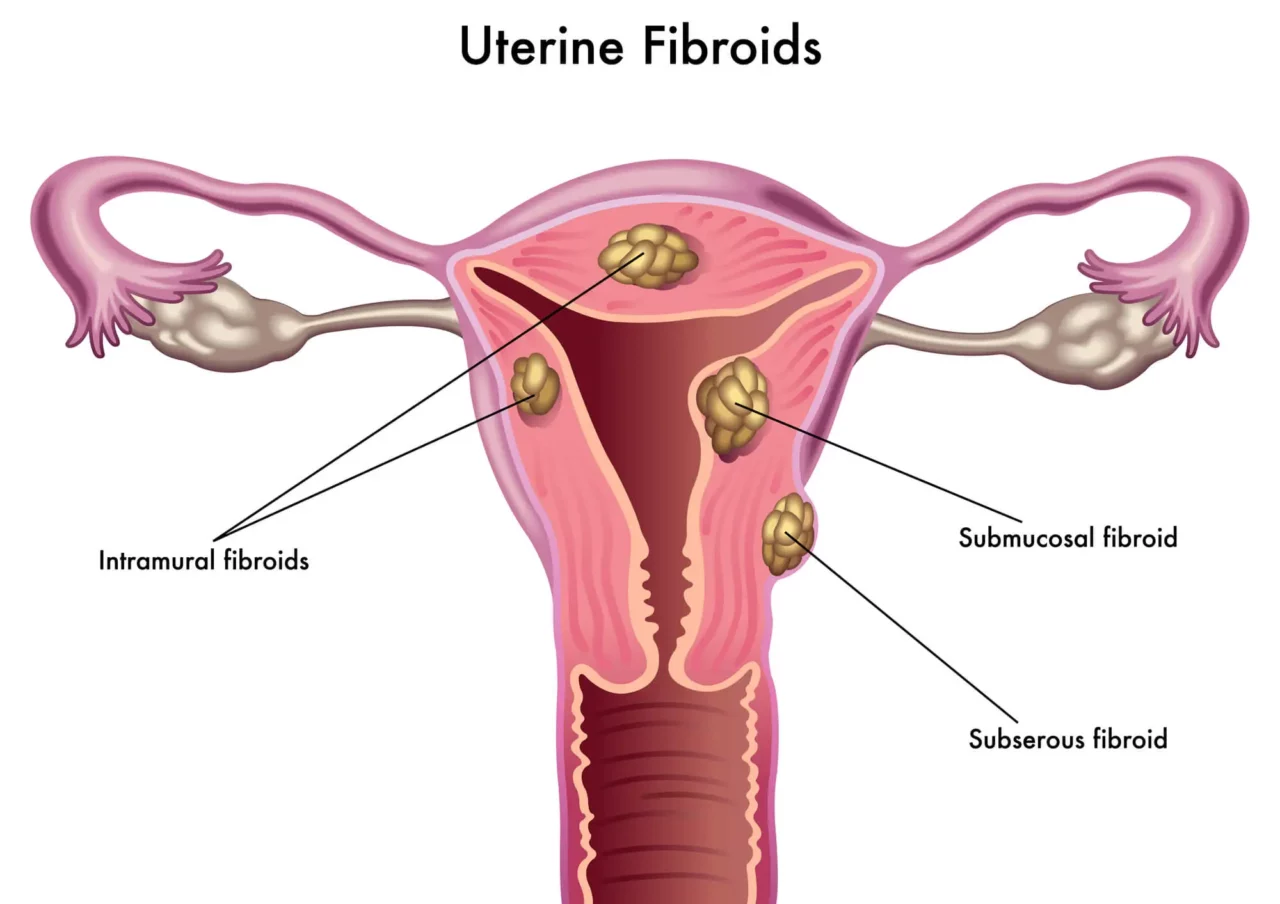
Fibroids
Fibroids, also known as myoma, are non-cancerous tumors that develop from muscle tissues within the womb and grow in or around the uterus, cervix, and fallopian tubes.
Fibroids may continue to grow over time and become very large, leading to severe consequences, including secondary dysmenorrhea and painful cramping. Other symptoms that indicate you may have fibroids in your uterus include having a bulging belly (as if you were pregnant), pressure on pelvic organs, frequent urination, and difficult bowel movements.
Although fibroids sometimes don’t cause symptoms, they should not be left unaddressed, as doing so can lead to problems during pregnancy and childbirth.
Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) is an inflammatory condition that affects a woman’s reproductive organs, including the uterus, fallopian tubes, and ovaries. PID is sexually transmitted and often develops as a complication of other STDs, such as chlamydia. Approximately 2.5 million women in the US have been diagnosed with this condition during their lifetime.
Besides dysmenorrhea, PID can cause pelvic pain, pain during sex, painful urination, bleeding between periods, heavy and painful periods, and abnormal vaginal discharge. Although this condition can be easily treated with a course of antibiotics, it is important not to let PID go unaddressed, as doing so can lead to infertility.
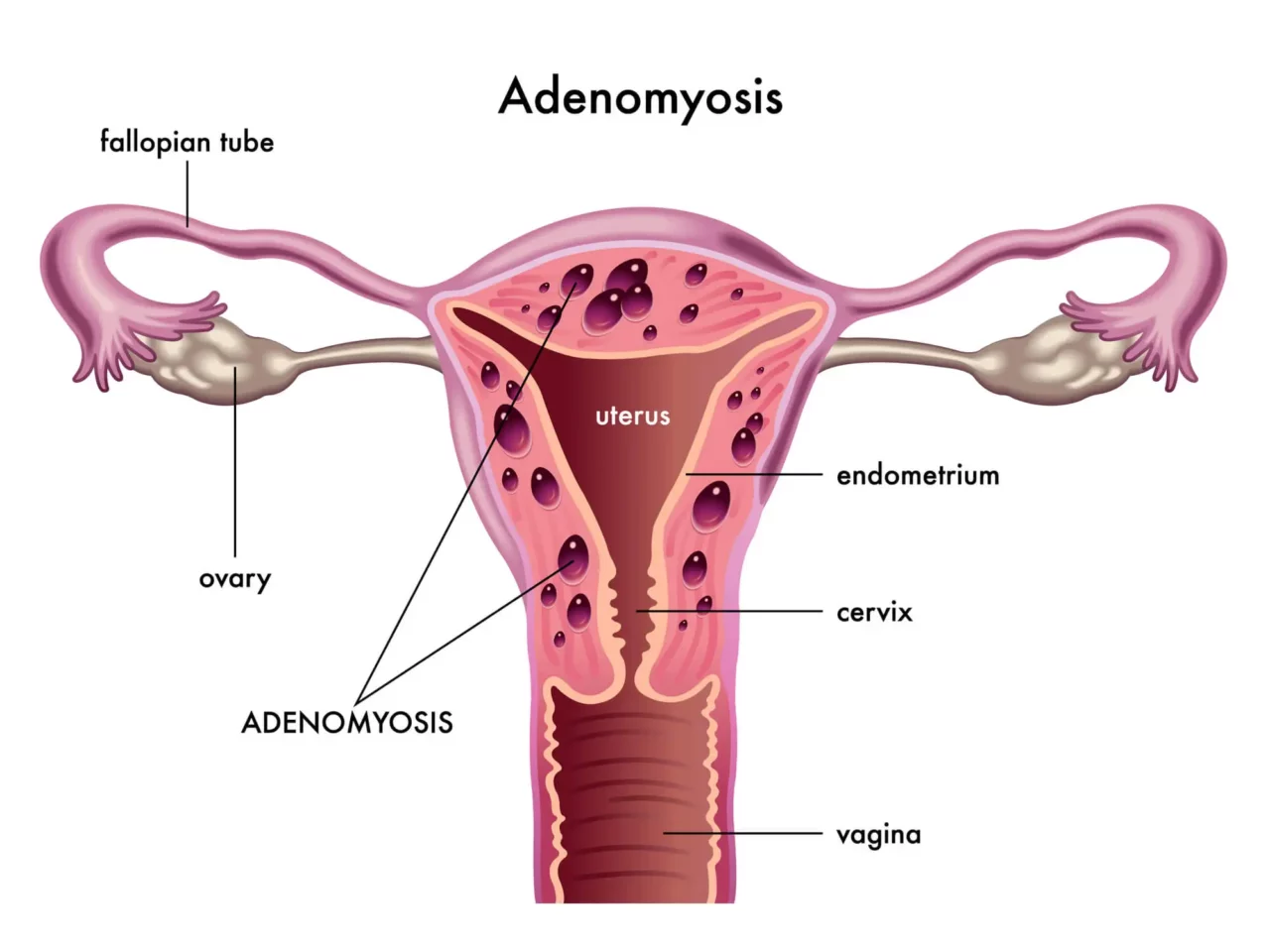
Adenomyosis
Adenomyosis is a condition that occurs when the endometrium (the lining of the uterus) grows into the muscular wall of the uterus. Similarly to endometriosis, these endometrial implants grow and thicken with each menstrual cycle but are unable to leave the body during menstruation. This leads to inflammation, pain, pressure, and an enlarged uterus. If you have adenomyosis, you may also experience dysmenorrhea and excessive bleeding.
Although adenomyosis can affect one in 10 women of reproductive age, the extent and severity of this condition vary from one person to another.
Cervical Stenosis
Cervical stenosis is a condition that causes the narrowing or closing of the passageway located in the lower part of the uterus, known as the cervix. This passageway is used by the menstrual blood to leave the body during menstruation. If the cervix is too small, it can slow down the menstrual flow, which increases pressure, pain, and inflammation inside the uterus during menstruation.
This condition also leads to menstrual abnormalities, infertility, hematometra (the accumulation of blood in the uterus), and, if the menstrual blood flows back into the fallopian tubes and ovaries, endometriosis.
Pain Conditions We Treat in NextPain Care
At NextPain Care, we specialize in treating a variety of pain conditions to improve your quality of life. Our expert team uses a comprehensive approach to address both physical and behavioral aspects of pain, ensuring you receive the best possible care. Here are some of the pain conditions we treat:
Risk Factors For Painful Menstrual Periods
Painful menstrual periods can affect any person who menstruates, at any point in their reproductive years. However, as outlined by a 2021 study, certain factors may increase your risk of suffering from this condition, including the following:
- Being under 20 years of age: Primary dysmenorrhea tends to decrease in intensity over time and disappears with menopause. If you suffer from this condition, painful symptoms associated with your period will begin to appear within a few months or years of your first period and improve significantly after the age of 40, even if you have never given birth to a child.
- Family history of painful periods: According to a 2014 study, having a family history of dysmenorrhea significantly increases the risk of developing this condition.
- Smoking: Smoking narrows the blood vessels, inhibits the supply of oxygen and nutrients to the reproductive organs, and increases inflammation. Additionally, smoking can influence hormonal activity, have toxic effects on the ovaries, and increase the risk of experiencing severe cramps that last two days or longer.
- Heavy bleeding with periods: If you have menorrhagia (heavy or prolonged menstrual bleeding), you are more likely to suffer from painful cramps because of the excessive cramping and prostaglandin secretion involved with menstruation. This condition may be caused by a range of conditions, including hormonal imbalances, dysfunction of the ovaries, and adenomyosis.
- Irregular periods: Irregular periods can put you at greater risk of suffering from dysmenorrhea. Periods that are both irregular and painful may be a symptom of another underlying condition, including endometriosis, polycystic ovarian syndrome (PCOS), or fibroids.
- Not experiencing pregnancy: Being nullipara, or never having given birth to a child, can increase your risk of experiencing painful periods. However, the pain should ease down after the age of 40.
- Reaching puberty before age 11: Early onset of menstruation may be associated with more painful periods, as well as conditions that cause secondary dysmenorrhea, such as endometriosis and fibrosis.
- Other risk factors for painful periods include drinking alcohol, several attempts to lose weight, a history of depression or anxiety, and disruption in your social or personal life.
When To Seek Medical Attention
No matter when you develop painful periods, dysmenorrhea can be a life-limiting condition that impacts all aspects of your life. For example, among adolescents, dysmenorrhea is a leading cause of school absenteeism, while adult women with painful menstrual cramps may be unable to work, participate in sports, or enjoy their hobbies.
But what’s even more concerning is the fact that painful periods may be caused by an underlying condition that, if left untreated, can lead to severe complications such as infertility. Because of this, knowing when to see a doctor for your painful periods is vital. Here are the telltale signs that should prompt you to see your doctor:
- Debilitating pain during periods: Whether you have primary or secondary dysmenorrhea, if the pain and discomfort you experience each month get in the way of your daily life, you should seek medical attention immediately.
- Chronic pain outside of menstruation: Chronic pain outside of menstruation or cramps that start several days before your periods and continue long after are a sign that you may be dealing with an underlying condition like endometriosis. A specialized doctor can help you obtain an accurate diagnosis.
- Painful sexual intercourse: Dyspareunia, or painful sex, is a condition that affects up to 18% of women. It can be caused by a wide range of conditions, including uterine fibroids, pelvic inflammatory disease, endometriosis, cystitis, irritable bowel syndrome, and ovarian cysts. If you are experiencing this symptom, a doctor can help you identify and treat the root cause of your pain.
- Ovarian cysts: Ovarian cysts are sacs filled with fluids that develop inside an ovary. This is a serious condition that causes symptoms such as swelling, bloating, pain in the pelvis, and painful sex.
- Infertility: Unexplained infertility may be caused by several conditions that are also the source of painful periods, including endometriosis, polycystic ovary syndrome (PCOS), and pelvic inflammatory disease (PID).
- Fever: When your body produces prostaglandins before your period, you may experience what’s known as “period flu,” or low-grade fever.
However, if your fever is rising, or accompanied by excessive bleeding, prolonged periods, and severe cramps, you should immediately see a doctor.
No response to pain medication or home remedies: Primary dysmenorrhea usually responds to anti-inflammatory non-steroidal medications and home remedies such as warm compresses. If your pain continues after your period or intensifies over time, you may be dealing with another underlying condition that requires medical attention.
Diagnosing Heavy, Painful Periods
As we have seen above, one of the leading causes of secondary dysmenorrhea is endometriosis. To provide you with an accurate diagnosis and a comprehensive clinical picture, your doctor may carry out the tests necessary to understand whether painful menstruation may be caused by endometriosis or another condition. These tests include the following:
- Complete blood count (CBC) test: A CBC with differential is used to determine the presence or absence of infections or other abnormalities. This type of test is recommended to all women, especially those aged 35 and above, even if they don’t experience significant problems.
- Lab cultures: Lab cultures are used to determine the presence or absence of sexually transmitted infections and diseases, such as chlamydia, that may be the source of painful periods.
- Laparoscopy: Laparoscopy is a surgical and diagnostic procedure that involves inserting a laparoscope (a thin viewing instrument) through small incisions performed around the pelvic area. The laparoscope can be guided to view the uterus, collect samples of tissues for testing, and remove abnormal growths that may be causing pain.
- Pelvic ultrasound: High-frequency sound waves can be used to obtain clear images of the inner pelvic area. This helps doctors determine the presence and extent of endometrial implants that may be causing pain.
Depending on your symptoms, a healthcare provider may also use imaging tests (i.e., MRI scans) to obtain a clear view of the presence, location, and severity of endometrial implants.
Managing Painful Menstrual Periods
Patients dealing with dysmenorrhea and endometriosis often face disbelief, dismissal, and the stigma surrounding menstruation. However, the pain from these conditions is real and debilitating.
Understanding the causes, symptoms, and prognosis of painful periods and endometriosis can help you see beyond daily medication to manage your pain effectively.
At NextPain Care, our multidisciplinary team integrates physical therapy and behavioral therapy into our three-tier comprehensive care system. Our approach is rooted in evidence-based practices, ensuring that our treatments are both effective and scientifically validated.
We prioritize starting with conservative measures such as physical therapy, lifestyle adjustments, and medication management to address your pain with minimal invasiveness. If these treatments prove inadequate, we explore advanced options like epidural steroid injections, nerve blocks, and spinal cord stimulation to provide more extensive relief.
We understand that living with pain can be challenging. We’re here to help with our distinctive approach to comprehensive care that addresses the multifaceted needs of our patients.
Start your journey to relieving period pain today.