Recognizing The Signs And Symptoms
Walking difficulties, also known as abnormal gait patterns, can result from various factors such as genetic conditions, traumatic injuries, or diseases affecting the muscles, bones, nerves, or ligaments in the legs, feet, or hips.
These conditions may affect specific parts of the leg, such as the knee, or involve the entire limb. Depending on the underlying cause, walking abnormalities can be acute and resolve with treatment, or chronic, leading to ongoing disability and challenges in daily activities.
There are several types of abnormal gait patterns that can cause walking difficulties:
- Scissor gait: Legs are slightly bent inward, and knees may cross or knock together during walking
- Propulsive gait: Characterized by a stooped, rigid posture with the head and neck thrust forward
- Steppage gait: Toes point downward, causing them to drag or scrape the ground even when the leg is lifted
- Waddling gait: Shifts weight from side to side or from one leg to another while walking
- Spastic gait: Involves dragging the feet or walking with stiffness
Other common gait abnormalities include irregular foot placements, unsteadiness, and involuntary or jerky movements. Gait issues resulting from nerve damage may resemble the walking pattern of a horse’s front legs.
If you are experiencing difficulties with walking, you may also notice accompanying symptoms such as the following:
Numbness And Tingling In The Legs And Feet
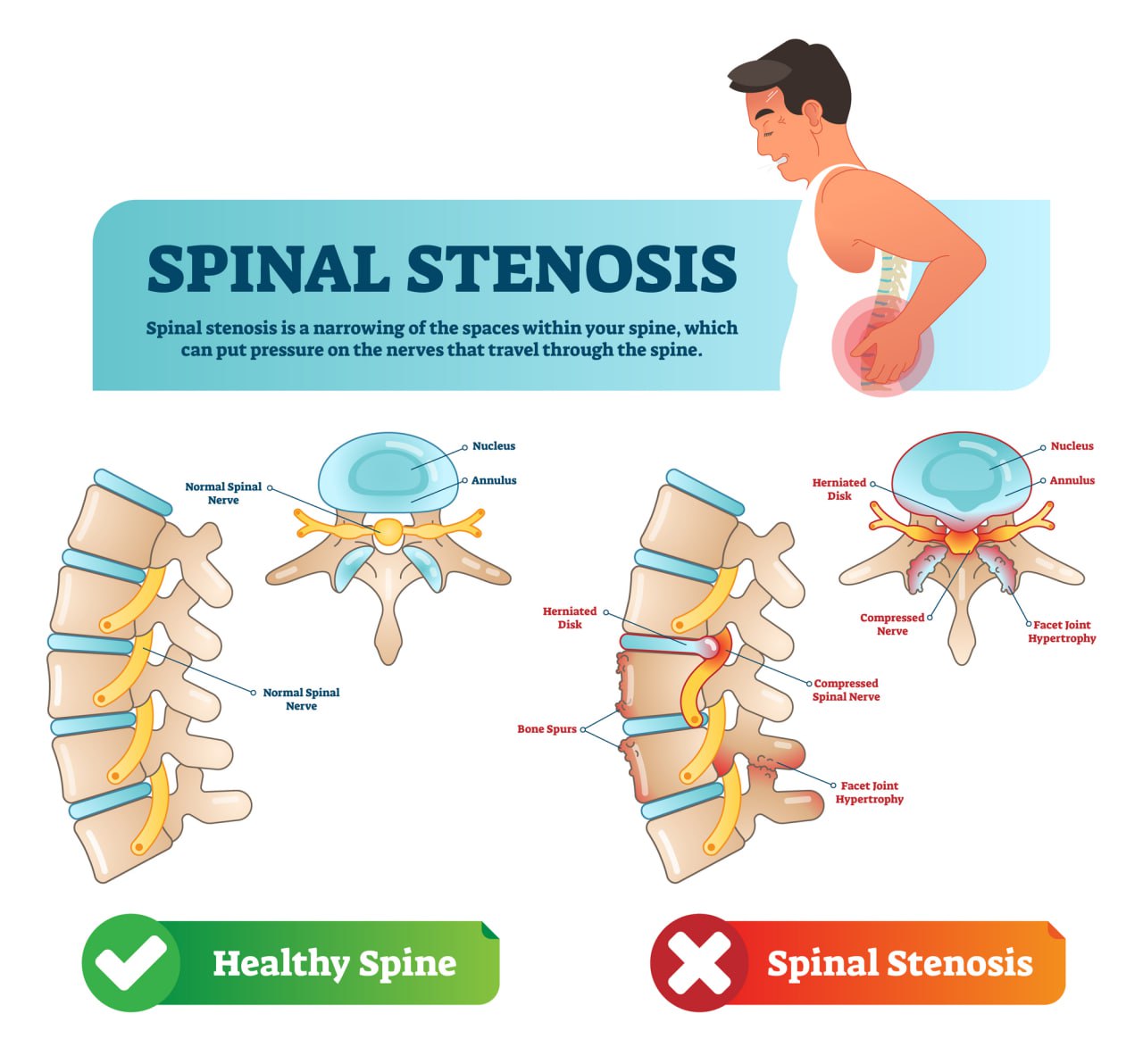
Numbness and tingling are sensations that occur when one or more nerves are irritated, damaged, or compressed. These sensations can result from conditions such as sciatica, spinal stenosis, or fibular nerve dysfunction.
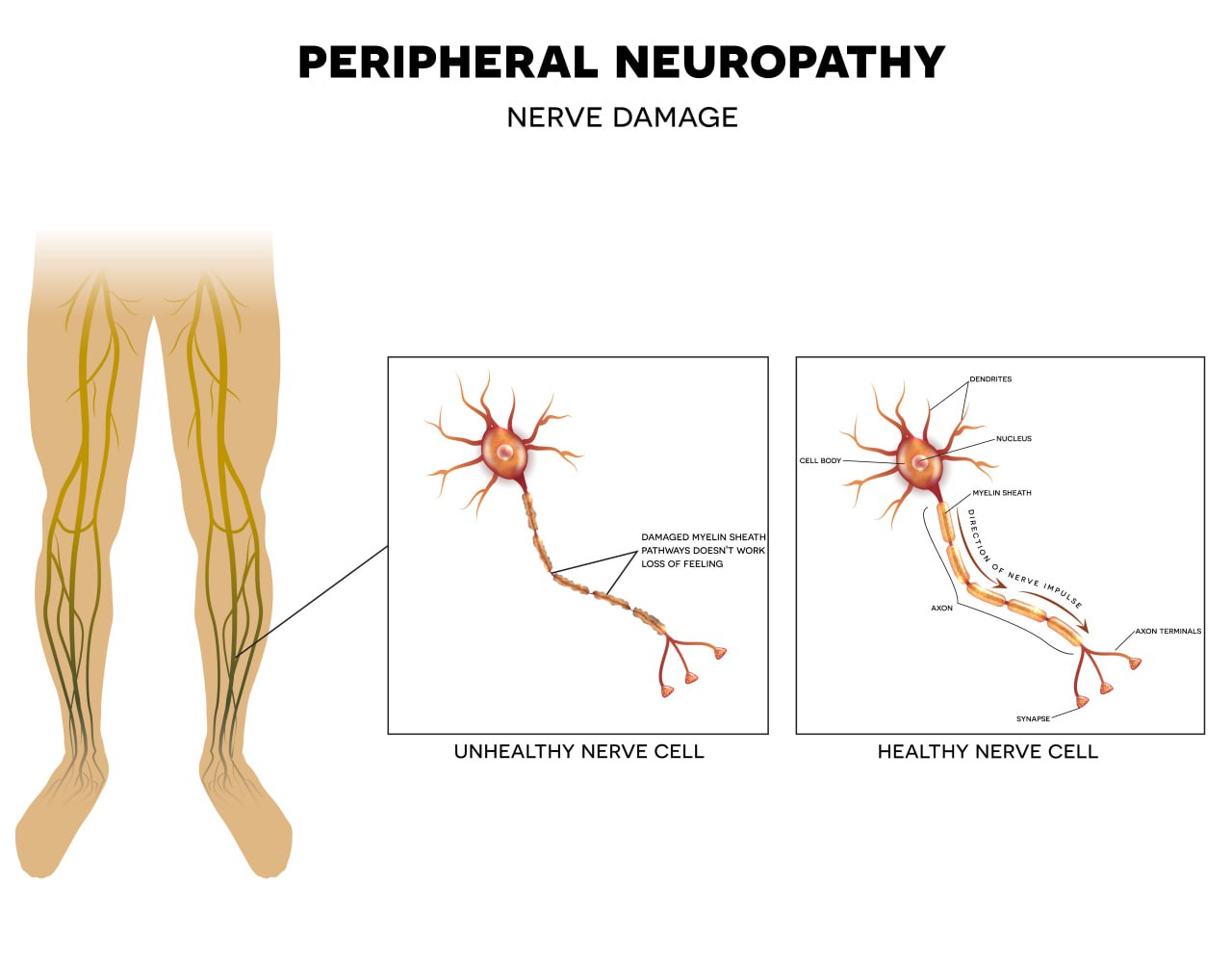
The peripheral nervous system, which consists of nerves outside the brain and spinal cord, is responsible for transmitting signals related to sensations and movement to and from the brain. When these nerves are compressed by other structures or damaged by disease, they may fail to deliver messages correctly regarding pain, temperature, touch, or muscle movement. This can also lead to involuntary firing of the nerves, causing sensations such as tingling, numbness, and “pins and needles,” also known as paresthesia.
Pain In The Hips And Lower Back
Pain in the hips and lower back is a non-specific symptom that can stem from various causes and risk factors. Poor posture and overuse, for instance, can strain muscles and exert undue pressure on certain components of the back.
Common health conditions associated with this type of pain, especially during walking, include sprains, strains, herniated discs, and sciatica. The interconnected nature of the vertebrae, joints, and nerves in the hips and lower back can explain why walking difficulties often come with pain in these areas.
Muscle Cramps
Experiencing muscle cramps in the legs can disrupt your ability to maintain a balanced, steady gait. Cramping muscles and spasms can increase the risk of falls and subsequent injuries, leading to ongoing disability.
Cramps are often linked to dehydration or temporary health events such as pregnancy and muscle fatigue. However, persistent or recurrent cramps that last for three months or more may indicate a more serious underlying condition, such as diabetes, kidney problems, or thyroid dysfunction.
Cramps and other involuntary muscle movements are also associated with conditions that affect the functioning of the nerves in the central and peripheral nervous systems, such as spinal stenosis and neuropathy. These disorders can interfere with the transmission of nerve signals related to movement, causing the nerve fibers within the muscles of the leg, foot, and hips to malfunction or fire up unexpectedly, leading to cramps and fasciculations (muscle twitches).
Muscle Weakness When Lifting The Feet Or Maintaining Balance
Muscle weakness, which can affect your gait and walking ability, may manifest when trying to lift your foot, move your leg forward, or maintain balance. This weakness can result from inactivity and a sedentary lifestyle, leading to reduced muscle conditioning, loss of muscle mass, and atrophy over time.
Studies have shown that muscle fatigue, particularly in the muscles supporting the ankle, is associated with decreased balance control in elderly individuals. In rare cases, muscle weakness can be caused by foot drop, a condition characterized by the inability to lift the forefoot while walking.
Foot drop results from weakness in the dorsiflexors of the foot, which are responsible for lifting the foot off the ground while walking. This condition can arise from muscular, neurologic, or musculoskeletal disorders, leading to an antalgic gait (a limp) that increases the risk of accidents and falls in the elderly.
Knee Joint Pain
Difficulty walking is often a symptom of musculoskeletal conditions that cause chronic pain, such as knee joint pain. Pain in the knee can make movements like bending your knee or climbing stairs challenging.
These abnormal movements can place undue pressure on other components of the lower body, such as the other leg, leading to mechanical issues, limping, and an abnormal gait.
Possible Conditions Contributing To Difficulty Walking
Not all forms of walking difficulties are the same or have the same causes.
Some walking challenges come naturally with age. Even if you remain active and fit, you may find it increasingly difficult to keep up the pace or climb stairs.
Although these changes are a normal part of aging, there are positive actions you can take to optimize your physical performance and decrease the risk of musculoskeletal conditions.
However, walking difficulties can also arise from specific conditions affecting mobility. These symptoms might begin after an injury, worsen over time, or become chronic (lasting three months or longer).
If you are struggling with chronic pain and reduced mobility, it is important to seek a treatment strategy to address the root cause and help you regain your normal gait. In such cases, you can’t simply “ride out” your symptoms. Taking medications may mask the pain, but the underlying problem will continue to progress over time.
Below, we’ll explore the most common conditions causing walking difficulties.
Injuries
Injuries affecting any part of the hip, leg, or foot can lead to walking difficulties and mobility issues.
- Traumatic injuries. These injuries occur from a direct blow or collision. Common traumatic injuries include fractures, joint dislocations, and ruptures, which involve the complete detachment of ligaments and tendons from the surrounding bones and muscles.
- Non-traumatic injuries. Non-traumatic and non-contact injuries often result from abnormal, sudden, or forceful movements. For example, twisting an ankle after landing from a jump or over-rotating a knee can overstretch ligaments and tendons or tear essential components of the joint, such as the meniscus.
Estimates show that the most common injuries affecting the lower extremities include sprains and strains (especially in the ankle) and fractures. These injuries can result from accidents, contact sports, falls at home, or poor form during physical activity.
These injuries are considered acute and can cause pain, joint instability, and the inability to bear weight on the affected leg. However, these symptoms should subside once the underlying cause is treated through immobilization and rehabilitation.
Spinal Stenosis
Joint Instability
Joint instability is a common condition that isn’t tied to a specific disease. Individuals may experience a sense of their joints feeling unstable or unable to support their body weight due to various factors.
For instance, if a tendon or ligament in the knee joint stretches beyond its capacity, it may fail to stabilize the surrounding bones and muscles during movement. This can result in sensations of the knee, hip, or ankle giving way, which can affect one’s gait.
Other contributing factors include:
- Osteoarthritis and conditions causing cartilage breakdown, impacting joint cushioning
- Genetic factors leading to hypermobile joints
- Overuse of joints
- Muscular imbalances or weakness
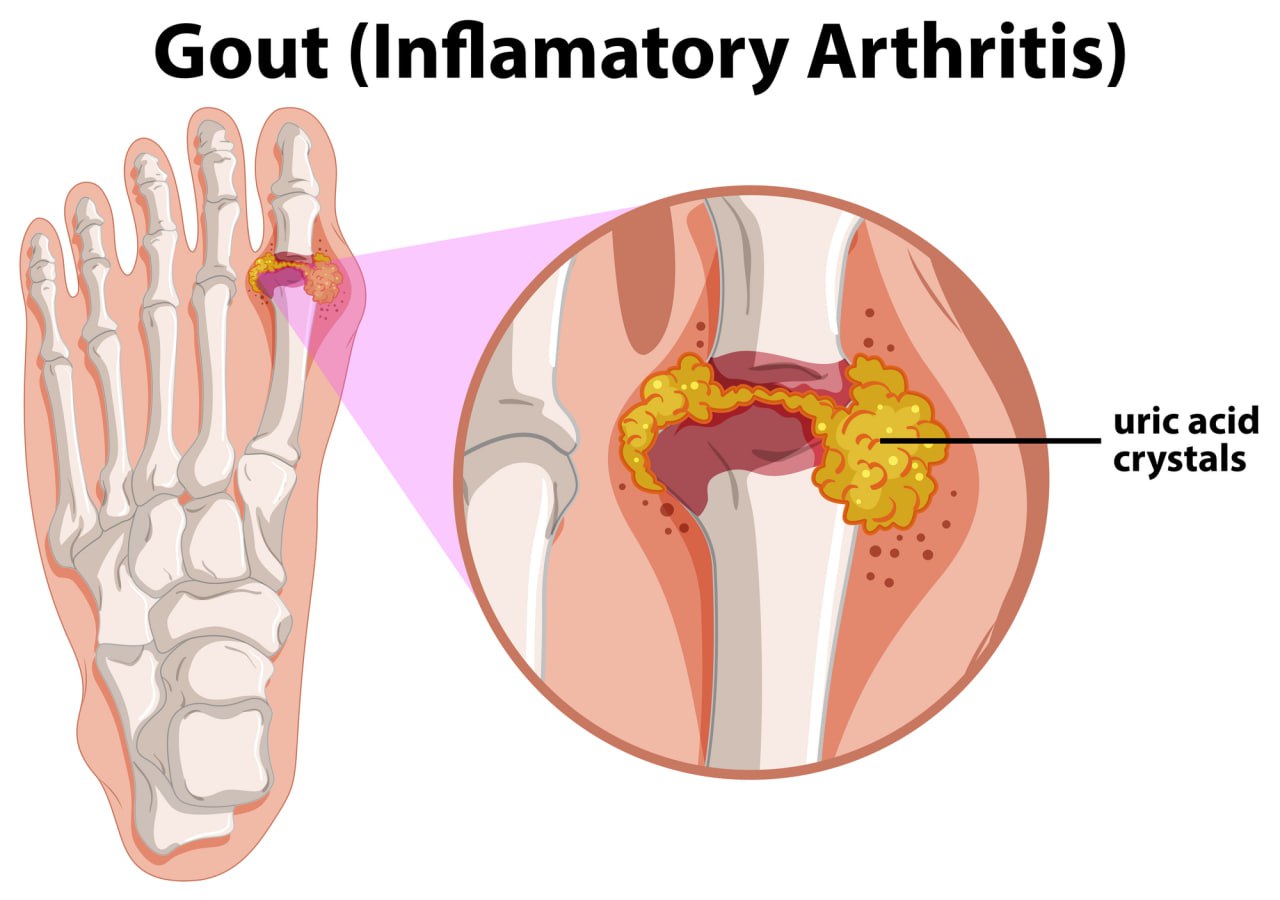
Gout
Gout is a type of inflammatory arthritis characterized by elevated levels of uric acid in the bloodstream. This excess uric acid can crystallize in joints or surrounding tissues, leading to inflammation and joint damage.
Initially affecting the big toe joint, gout causes severe pain, swelling, and redness. Over time, the accumulation of urate crystals can contribute to cartilage degeneration and bone damage in affected joints, potentially leading to mobility issues.
Several factors contribute to the development of gout, including a diet high in purine-rich foods (such as meat and alcohol), obesity, certain medications, and kidney disease.
Apart from the big toe, gout commonly affects joints like the ankles and knees, significantly increasing the risk of walking difficulties. During gout flare-ups, individuals often find it challenging to stand or walk, although gentle movement may offer some relief. Studies indicate that people with a history of gout typically exhibit slower walking speeds and perform poorly on tests assessing mobility, chair stands, and balance.
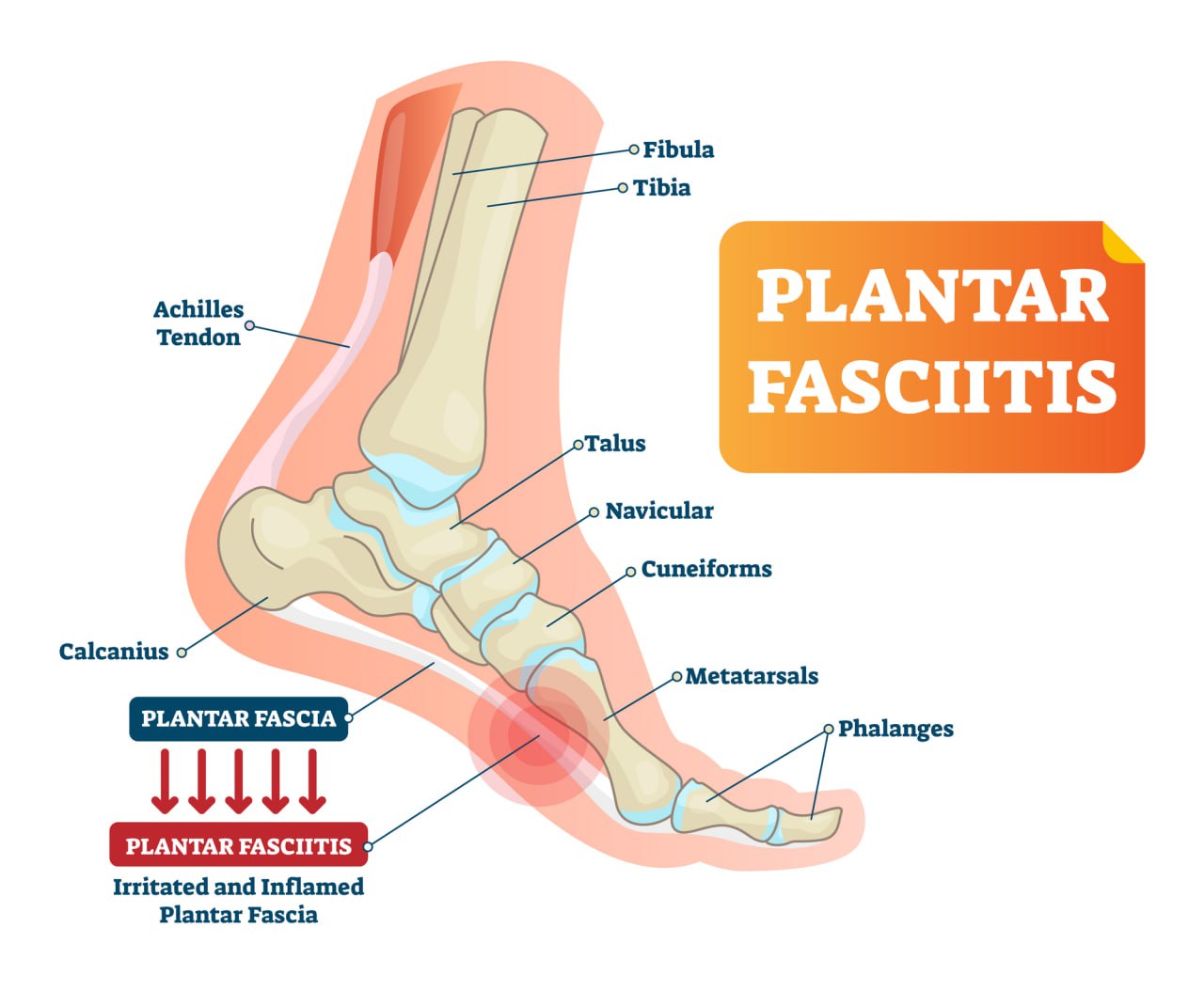
Foot And Ankle Problems
Walking difficulties can stem from deformities and inflammatory conditions affecting the ankle or foot, altering gait mechanics or causing discomfort during movement. Several prevalent conditions that can impact your walking include:
The plantar fascia is a robust band of collagen fibers that connects the heel to the toes, providing essential support for the foot arch, shock absorption, and facilitating foot movements.
When inflamed or damaged, plantar fasciitis or plantar heel pain (PHP), results in pain and restricted mobility. Causes include overuse, repetitive high-impact activities, foot abnormalities like flat feet, or changes in physical activity levels. Untreated, it can worsen, leading to increased inflammation, pain, and potential tearing of the fascia.
- Achilles tendonitis
- Foot deformities
Musculoskeletal Disorders
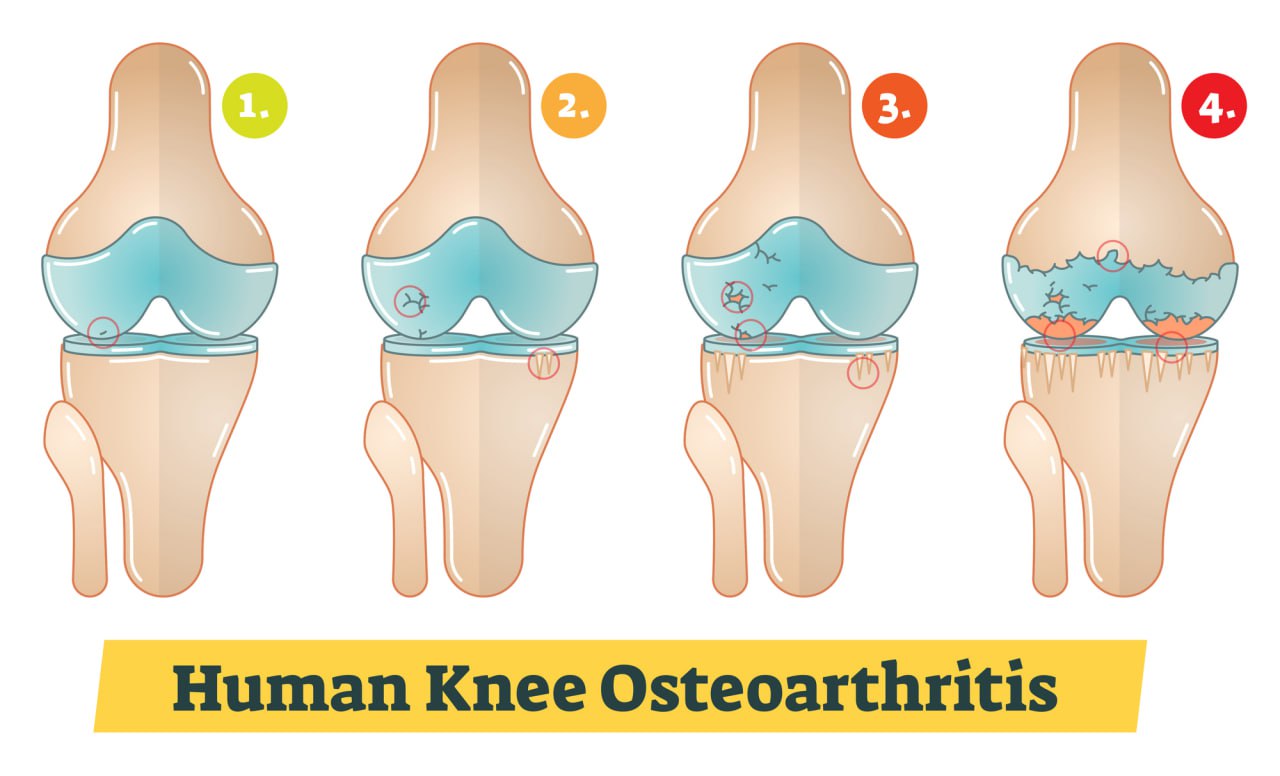
Common musculoskeletal disorders – acute or chronic – leading to walking difficulties include:
Rheumatoid arthritis (RA) is an inflammatory autoimmune disease that arises when the immune system mistakenly attacks healthy tissues, such as cartilage in the joints. This condition results in swelling and pain, particularly affecting the knees and feet.
Although RA can affect individuals of any age, it is most prevalent among women aged 40 to 60. In the United States alone, over 1.3 million people are currently affected by RA.
Common symptoms of RA include joint stiffness, chronic pain, and tenderness, which are caused by high levels of systemic, uncontrolled inflammation throughout the body. RA can also cause pain and swelling in the ankles and feet, making standing, walking, and performing everyday movements difficult.
As the cartilage wears down, a variety of symptoms may develop, including pain, swelling, and joint stiffness. Over time, the altered movement mechanics and high levels of inflammation can lead to complications such as bone damage and the formation of bone spurs.
Given these symptoms, it’s not surprising that OA can severely impact mobility, resulting in an abnormal gait, limited range of motion, and an increased risk of falls. OA is one of the most common chronic conditions in America. It is not only the most prevalent form of arthritis but also a leading cause of disability among the elderly.
- Fractures
- Sprains and strains
Sprains and strains are very common conditions that occur when a tendon or ligament is stretched beyond its capacity or in an awkward direction. They can result from dislocations or fractures, but are also frequently caused by rolling or twisting an ankle.
These injuries lead to pain, inflammation, and, in severe cases, an inability to bear weight on the affected joints. Individuals involved in sports such as soccer and football are at high risk for severe ligament and tendon injuries, including ACL tears in the knee.
Like fractures, sprains and strains are acute conditions that can be treated by allowing the affected ligament or tendon to heal. However, if proper healing does not occur, the pain can become chronic, impacting long-term mobility and sports performance.
Neurological Disorders
Neurological disorders can affect any part of the central nervous system (the brain and spinal cord) and the peripheral nervous system (nerves throughout the body outside of the brain and spinal cord).
These disorders disrupt the transmission of signals related to movement, sensations, and autonomic functions (such as heartbeat, digestion, and blood pressure) between the brain and other parts of the body.
Symptoms of neurological disorders vary depending on the affected areas of the nervous system, but they generally worsen over time if left untreated. Some of the most common neurological disorders impacting mobility include:
- Multiple sclerosis (MS)
MS is a chronic, debilitating disease that affects the central nervous system. It occurs when the immune system mistakenly attacks the myelin sheath, the protective layer surrounding nerve fibers in the brain and spinal cord. This damage disrupts the transmission of nerve signals, leading to a wide range of symptoms. While MS can affect individuals of any age, it most commonly targets adults between 20 and 50 years old.
The symptoms of MS vary widely, from mild numbness in the limbs to severe paralysis and vision loss. Mobility issues, such as difficulty walking or maintaining balance, are frequent due to muscle weakness and spasticity. These mobility challenges can significantly impact daily life and overall quality of life.
- Parkinson’s disease
Parkinson’s Disease is a progressive neurological disorder that severely impacts motor functions. It is caused by the degeneration of neurons in a specific area of the brain responsible for producing dopamine, a neurotransmitter crucial for coordinating movement. As these neurons die off, dopamine levels decrease, leading to a range of motor symptoms.
The hallmark symptoms of Parkinson’s include tremors, muscle rigidity, bradykinesia (slowed movements), and postural instability. These symptoms progressively worsen over time, making it increasingly difficult to walk, maintain balance, and perform everyday activities. Parkinson’s disease significantly impairs mobility and can drastically reduce a person’s independence and quality of life.
The tarsal tunnel is a narrow space in the ankle through which the posterior tibial nerve travels. Tarsal Tunnel Syndrome occurs when this nerve becomes compressed or pinched within the tarsal tunnel, causing pain and discomfort in the foot and ankle.
Symptoms can vary based on the extent of the compression and the specific nerves affected, but they often include numbness, tingling, and a reduced ability to sense pain or temperature changes in the affected area.
- Stroke
A stroke occurs when blood flow to a part of the brain is interrupted, either due to a blood clot blocking the flow or a blood vessel bursting or leaking in the brain. Although it primarily affects the elderly, strokes can occur at any age.
Symptoms of a stroke often appear suddenly and may include facial drooping, arm weakness, and difficulty with speech. If left untreated, a stroke can lead to severe disability or even death. After a stroke, many individuals face challenges with walking, often due to impaired nerve signaling, muscle weakness, and coordination issues.
- Spinal cord injuries
The spinal cord functions as a “highway” for nerve signals traveling to and from the brain, playing a crucial role in processing certain signals and enabling functions such as movement and sensation.
Spinal cord injuries can result from traumatic events, such as accidents or spinal fractures, but may also occur due to surgical injuries, sports accidents, or diseases. These injuries can severely impact the ability to move and feel, depending on the location and severity of the damage.
Peripheral Artery Disease (PAD)
Lifestyle Factors Affecting Mobility And Walking
Your lifestyle plays a crucial role in determining the risk of walking difficulties and mobility issues. Fortunately, many of these factors are modifiable, and adopting simple yet effective strategies can help you reduce the risk of mobility problems.
Let’s look at the main factors to focus on:
- Obesity or excess weight. Carrying excess weight, indicated by a high Body Mass Index (BMI), can place significant stress on the lower limbs and joints. This increases the risk of developing mobility-reducing conditions such as osteoarthritis. Additionally, obesity is a major risk factor for cardiovascular disease, stroke, diabetes, and peripheral neuropathy.
- Sedentary lifestyle. Leading a sedentary lifestyle can result in muscle weakness and poor circulation, which can contribute to weight gain. These factors elevate the risk of circulatory issues, muscle atrophy, falls, and fractures, all of which can impair mobility.
- Inactivity after surgery or injury. Extended periods of inactivity or bed rest following surgery or injury can negatively affect the musculoskeletal system, leading to muscle wastage and reduced circulation of essential blood, oxygen, and nutrients to the limbs.
- Alcohol and substance abuse. The abuse of alcohol, nicotine, and other substances can have neurotoxic effects, damaging nerves and increasing the risk of peripheral neuropathy. Alcohol abuse can also impact brain health and contribute to conditions like diabetes.
- Stress and fatigue. Chronic stress and muscle fatigue can exacerbate systemic inflammation, worsening conditions such as arthritis, osteoarthritis, tendinitis, and plantar fasciitis.
When To Seek Medical Help
How To Handle Walking Difficulties
Gait abnormalities may resolve naturally when the underlying cause is addressed. For instance, if your walking difficulties stem from a fracture or ligament tear, you can expect to regain a healthy gait once the injury heals.
However, for inflammatory or chronic conditions, healthcare professionals may recommend a variety of treatment strategies, including:
- Medical treatments. Healthcare providers might prescribe medications to alleviate symptoms while the injury heals or to treat infections. For chronic conditions like diabetes or multiple sclerosis, ongoing treatments may be necessary.
-
-
- NSAIDs – Non-steroidal anti-inflammatory medications, such as aspirin and ibuprofen, work by blocking the COX enzyme, which is involved in producing prostaglandins. This leads to a reduction in pain and inflammation.
-
- Physical therapy. Physical therapy is crucial for recovery post-injury, surgery, or illness. It helps patients restore an ideal gait and counteracts the effects of leg or foot deformities.
- Assistive devices. Assistive devices can reduce disability in progressive diseases or aid recovery. Common devices include:
- Canes
- Walkers
- Wheelchairs
- Lifestyle modifications. Lifestyle changes can significantly reduce the risk of walking difficulties. Patients should consider:
- Increasing physical activity
- Avoiding alcohol and nicotine
- Optimizing diet
- Managing stress, rest, and sleep
- Surgery. Surgery might be an option if other treatments fail or if walking difficulties severely impact independence. Surgical interventions aim to restore joint function, relieve compressed nerves, or repair joint damage.
While these treatment strategies can help manage symptoms, they often involve extended rehabilitation periods.
Does that mean you’ll have to live with walking difficulties forever? Fortunately, no. Let’s explore the solutions below.
The NextPain Care Approach To Walking Discomfort And Limitation
Conditions Associated With Difficulty In Walking Managed At NextPain Care
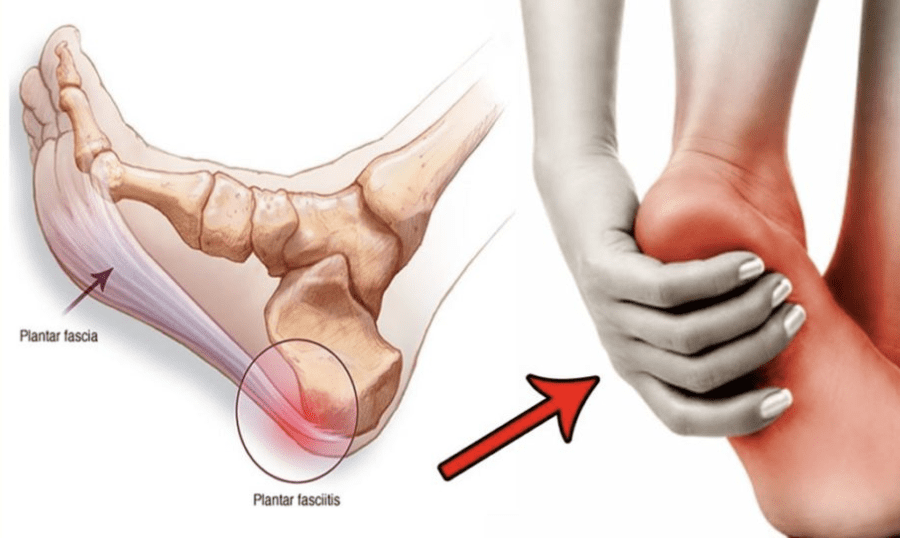
Plantar Fasciitis Pain Treatment
NextPain Care provides pain management for plantar fasciitis, focusing on improving mobility and offering lasting relief from chronic heel pain through personalized...

Rheumatoid Arthritis Pain Treatment
Rheumatoid arthritis can be a debilitating and painful condition that causes swelling, joint damage, and immobility. NextPain Care offers a comprehensive approach to treating the pain associated with rheumatoid arthritis and the condition itself. We aim to...

Peripheral Neuropathy Treatment
Peripheral neuropathy is a condition that can cause severe pain, impacting daily life. At NextPain Care, we use evidence-based practices to provide relief from the painful symptoms of peripheral neuropathy, adhering to the highest standards set by medical...
Journey To Better Mobility Starts Here
Find out how NextPain Care can help alleviate your walking discomfort and enhance your daily life.