Fibromyalgia is a condition characterized by chronic pain throughout the body, fatigue, anxiety, and nerve dysfunction. Affecting over 4 million people in the US, untreated fibromyalgia can lead to disability. While there is no definitive cure, treatments aim to alleviate symptoms.
Despite its prevalence and debilitating nature, fibromyalgia’s “invisible” nature has delayed research on its causes, symptoms, and prognosis. Clinical trials only began in the 1980s, and much remains to be understood.
One emerging hypothesis is that fibromyalgia is an autoimmune disease, a condition caused by the immune system mistakenly attacking healthy cells. While this theory is not widely accepted by the international scientific community, new research could pave the way for better understanding and treating fibromyalgia.
This guide explores the potential connection between fibromyalgia and autoimmunity, and non-pharmacological approaches to managing the condition.
The Link Between Fibromyalgia And Autoimmunity
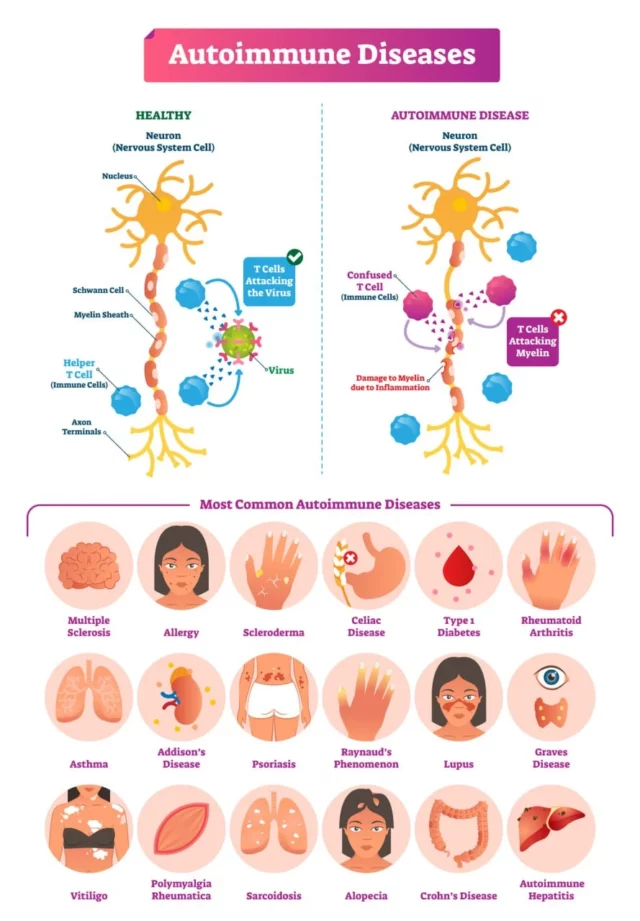
To consider fibromyalgia as an autoimmune disease, it’s important to understand autoimmunity, where the immune system mistakenly attacks healthy tissues, causing sustained inflammation and progressive damage.
Common autoimmune conditions include Crohn’s disease, type 1 diabetes, rheumatoid arthritis, lupus, and multiple sclerosis. These conditions have no cure, and treatments typically focus on managing symptoms.
For a disorder to be classified as an autoimmune disease, it must exhibit certain hallmarks:
- Damage to tissues by the immune system
- Sustained inflammation
- Presence of autoantibodies
Autoantibodies are proteins produced by the immune system that mistakenly attack healthy cells. For instance, the autoantibody anti-dsDNA is linked to lupus, while anti-CCP is associated with rheumatoid arthritis.
Research must confirm these hallmarks for fibromyalgia to be considered an autoimmune disease. However, fibromyalgia has historically been controversial and often misclassified as “generalized musculoskeletal pain,” due to inadequate diagnostic tools.
Fibromyalgia shares several similarities with autoimmune diseases:
- Higher prevalence in women
- Development following trauma or disease
- Increased risk with pathogens like Hepatitis C
- Co-occurrence with other autoimmune diseases
- Post-vaccination or medical event onset
New research also highlights hallmarks of autoimmunity in fibromyalgia:
- Autoantibodies: Found in some patients with fibromyalgia
- Inflammation: High levels of inflammatory proteins are present in fibromyalgia patients
- Damage: Associated with small-fiber neuropathy
Additionally, fibromyalgia features increased pain-related brain activity linked to abnormal neuroinflammation.
The Role Of Genetics And The Immune System
Although the hypothesis linking fibromyalgia to autoimmunity is not widely accepted, genetics and the immune system play significant roles. Symptoms like fatigue and pain sensitivity are linked to overactivity in pain-sensing nerves, often following an infection or injury.
Genetics also influence fibromyalgia risk. Having a close relative with an autoimmune disease or fibromyalgia increases your risk.
Does Fibromyalgia Weaken The Immune System?
When the immune system experiences severe trauma or responds to injury or infection (e.g., Hepatitis C), it can start to malfunction. A malfunctioning immune system may produce autoantibodies that lead to autoimmune diseases, or it can become overactive, increasing the activity levels of pain-sensing nerves.
These consequences can lead to the development of autoimmune diseases and chronic pain conditions like fibromyalgia. Conversely, having fibromyalgia can weaken the immune system.
Studies have shown that patients with fibromyalgia have high counts of pro-inflammatory cytokines (immune cells), which cause sustained inflammation. Chronic inflammation can disrupt the functioning of the immune system, leading to autoimmune diseases and allergies.
Over time, widespread inflammation can also cause a cascade of complications, such as damaging healthy tissues, including cartilage and myelin (the nerves’ protective sheath). Additionally, when the immune system is constantly involved in the inflammatory response, it may not correctly fight off harmful bacteria and viruses.
Ongoing inflammation can also interfere with essential bodily functions, including digestion and sleep. A lack of appetite or sleep disturbances can further weaken the immune system and facilitate the development of illnesses.
Studies from 2020 also indicate that fibromyalgia can be considered a low-cortisol state. Lower cortisol concentrations are associated with higher pain intensity, a symptom of fibromyalgia. Cortisol is a hormone responsible for regulating the stress response and the levels of estrogen in the body. Low cortisol levels cause estrogen levels to drop, which is associated with higher levels of progestin, a hormone that inhibits immune functions.
Over time, hormone fluctuations and chronic inflammation can compromise the immune system, increasing the likelihood of developing other diseases and health conditions.
Challenges In Diagnosing Fibromyalgia As An Autoimmune Disease
Diagnosing fibromyalgia is challenging due to its “invisible” symptoms and lack of identifiable causes. It shares symptoms with other conditions, complicating diagnosis.
While the body of research is growing, more is needed to fully understand and classify fibromyalgia as an autoimmune disease.
Difficulty In Identifying Common Symptoms And Causes
One of the main reasons fibromyalgia remains challenging to diagnose is the difficulty healthcare providers face in identifying its symptoms and causes.
Despite the growing body of research since the 1970s, many patients today must deal with a condition with no identifiable cause. Current hypotheses suggest that fibromyalgia may be caused by abnormalities in the immune system’s functioning or by interference with how the brain processes pain signals.
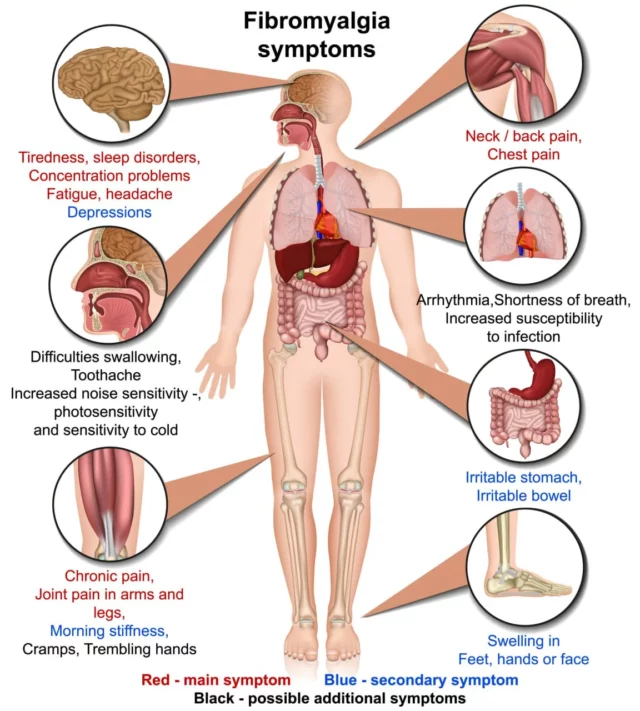
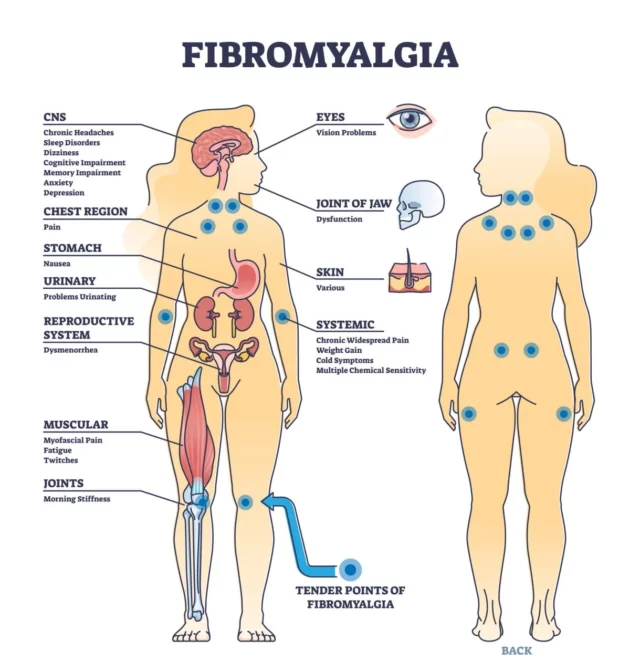
For patients at greater risk of fibromyalgia, the condition often begins after other health events, such as trauma, injury, illness, or mental health issues like depressive episodes. The symptoms of fibromyalgia are just as challenging to identify as its causes.
Patients frequently experience widespread musculoskeletal pain, stiffness, fatigue, tiredness, anxiety, memory problems, and headaches. These symptoms not only overlap with conditions like chronic fatigue syndrome but also resemble other autoimmune diseases such as rheumatoid arthritis.
Conventional Treatment Options For Fibromyalgia
While there is no definitive cure for fibromyalgia, there are several treatment options available to help manage its symptoms. These treatments focus on improving quality of life by reducing pain, enhancing sleep, and increasing overall well-being.
Here are some of the conventional treatment options:
Lifestyle Changes
Making certain lifestyle changes can significantly help in managing fibromyalgia symptoms. These changes include:
- Education: Learning about fibromyalgia can help patients understand their condition better and find effective ways to manage it.
- Improved sleep: Establishing a regular sleep routine and creating a restful sleep environment can help reduce fatigue and improve overall health.
- Physical activity: Engaging in regular physical activity, such as walking, swimming, or gentle stretching exercises, can help reduce pain and improve mood.
Medications
Several types of medications can be prescribed to help manage the symptoms of fibromyalgia. These medications include:
- Nonsteroidal anti-inflammatory medications (NSAIDs): These medications can help reduce pain and inflammation.
- Anti-seizure medications: Originally developed to treat epilepsy, these medications can help reduce certain types of pain associated with fibromyalgia.
- Antidepressants: These medications can help improve mood and reduce pain by affecting neurotransmitters in the brain.
- Muscle relaxants: These medications can help relieve muscle tension and improve sleep.
Physical And Occupational Therapies
Engaging in physical and occupational therapies can provide significant relief for fibromyalgia symptoms. These therapies include:
- Tailored exercise programs: These programs are designed to meet the specific needs of individuals with fibromyalgia, helping to improve strength, flexibility, and endurance.
- Massage therapy: Regular massage can help reduce muscle tension and improve circulation, leading to reduced pain.
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific points on the body to reduce pain and promote healing.
- Stress management techniques: Learning and practicing stress management techniques, such as deep breathing exercises, meditation, and mindfulness, can help reduce the impact of stress on the body and improve overall well-being.
Pain Management At NextPain Care
NextPain Care follows a structured three-level system to manage fibromyalgia and other chronic pain conditions effectively. This approach begins with conventional therapies, including physical therapy, stress management techniques, and lifestyle changes like balanced nutrition and regular physical activity.
If needed, the second level introduces medication management, carefully tailoring prescriptions to alleviate symptoms while minimizing side effects. The final level focuses on minimally invasive procedures, designed to disrupt pain signals and stimulate the body’s natural healing processes, providing significant relief for patients when conventional methods are insufficient.
By integrating these three levels, NextPain Care offers a comprehensive, personalized treatment plan that supports long-term well-being.
Pain Shouldn’t Stop You From Living Your Best Life
NextPain Care prioritizes starting with non-invasive procedures, advancing to minimally invasive treatments and then to more comprehensive options, as needed. This approach ensures that patients receive the most appropriate care based on their specific condition and symptoms.
By focusing on a step-by-step approach, NextPain Care provides effective and personalized treatment plans that cater to the unique needs of each patient.
We understand that living with chronic pain can be physically, emotionally, and socially challenging. That’s why we strive to not only address the pain symptoms but also improve the overall quality of life for our patients.
You don’t have to suffer in silence and miss out on living your best life. Let NextPain Care help you find the relief and support you need to thrive and enjoy every day.
You don't have to face fibromyalgia alone. We can help.

