Endometriosis is a chronic inflammatory condition that impacts over 6.5 million women in the US. Each person with endometriosis may experience it differently. Some might have mild symptoms, while others may experience severe pain, heavy bleeding, and infertility.
More than half of those with endometriosis also suffer from significant leg pain. Though often seen as a secondary issue, leg pain can be severe, spreading to the buttocks, leg, and foot, leading to mobility problems, reduced work performance, and disability, profoundly affecting one’s life.
Misdiagnosis and poor management often exacerbate endometriosis-related leg pain. However, much can be done without relying on medications or surgery.
Our methodologies can do more than just reduce pain; it can equip you with practical tools to manage your condition and improve your quality of life. Let’s delve into the essential details.
Can Endometriosis Be A Source Of Leg Pain?
Understanding how endometriosis leads to leg pain is still evolving. However, recent research has started to clarify this link. To comprehend the connection, we must first understand endometriosis itself.
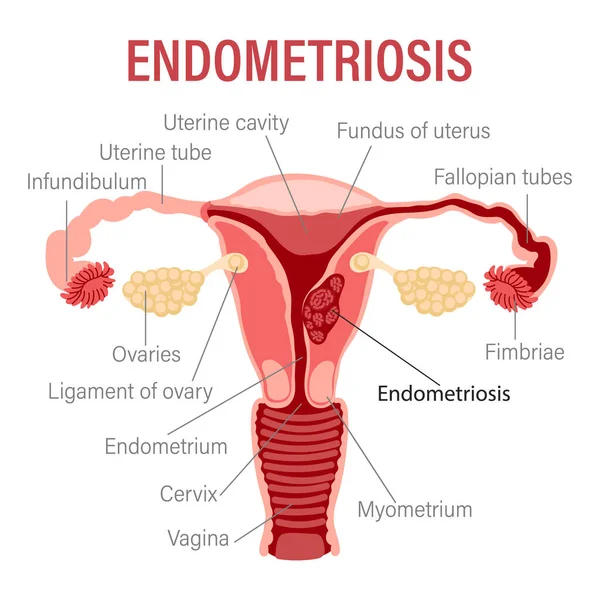
The uterus, or womb, is a pear-shaped organ in a woman’s pelvis that plays a role in menstruation, gestation, and labor. The uterus is lined with endometrial tissue, which grows and thickens during the menstrual cycle to prepare for a fertilized egg.
During early pregnancy, the endometrium provides the fertilized egg with oxygen, nutrients, and protection necessary for fetal development. If no egg is fertilized, the body sheds the endometrium through menstruation. This cycle of growing and shedding endometrial tissue repeats monthly.
Endometriosis occurs when this endometrial tissue grows outside the uterus, forming endometrial implants. These abnormal growths cause severe inflammation, cysts, scarring, and adhesions, binding the pelvic organs together.
If left untreated, these complications can disrupt organ function and lead to infertility, affecting 30-50% of women with endometriosis.
Endometrial implants can spread to the organs and tissues around the uterus, including:
- Exterior walls of the uterus
- Ovaries
- Fallopian tubes
- Bladder
- Rectum
- Cervix
- Pelvic cavity
- Vagina
- Nerves near the uterus
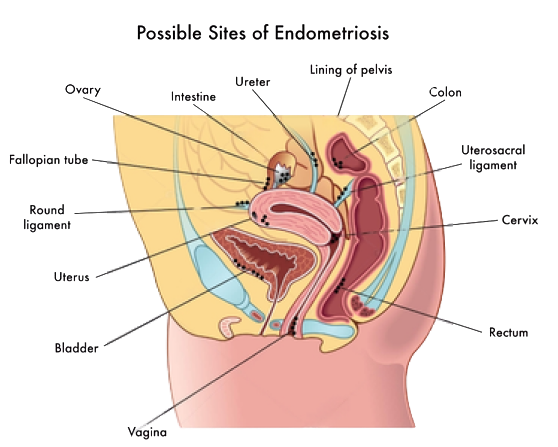
This leads to an abnormal buildup of endometrial tissue, which can cause blood to get trapped in the ovaries, block fallopian tubes, create adhesions between organs, and form scar tissue on reproductive organs.
The most common symptoms of endometriosis include severe pain during menstruation and intercourse, nausea, vomiting, heavy bleeding, pelvic pain, and pain when urinating or passing stools. In some cases, it can also cause leg pain.
Leg pain from endometriosis occurs when nerves near the uterus and other pelvic organs become inflamed, compressed, or damaged. This affects the transmission of motor and sensory signals to and from the brain.
This can cause pain, numbness, and tingling sensations. These symptoms can result from:
- Endometrial implants on pelvic nerves, such as the sciatic or obturator nerves, cause scarring and lesions.
- Inflammation affects nearby organs and tissues, leading to swelling and nerve compression.
- Inflammation impacts blood vessels, reducing blood flow and nutrient supply to nerves, causing damage or death of nerve fibers.
- Genetic factors may contribute to endometriosis, but there is no specific “endometriosis gene.”
Understanding these factors can help manage the condition and improve the quality of life for those affected by endometriosis.
What Does Leg Discomfort From Endometriosis Feel Like?
Leg pain can be hard to diagnose because it is non-specific. It’s even more challenging to determine if this pain comes from endometriosis.
However, understanding what leg pain from endometriosis feels like is important. This way, you can seek the right diagnosis and avoid taking medications that only mask symptoms and cause side effects.
Knowing when your symptoms are linked to endometriosis is crucial, especially since about 90% of people with this condition are not believed or are dismissed by healthcare providers and loved ones.
Leg pain from endometriosis is often described as stabbing or throbbing, and it gets worse during menstruation when the endometrial implants grow and thicken.
This pain feels different from regular muscle cramps or soreness and might come with a pulling sensation in the leg, tingling, numbness, or heaviness. The pain can be so severe that it prevents walking or physical activity, causing serious mobility issues for days each month.
Other symptoms include:
- Difficulty walking
- Loss of muscle mass
- Sleeping problems and interrupted sleep due to pain
- Trouble sitting for long periods
- Restless legs syndrome (RLS)
Heaviness In The Legs
When nerves around the uterus are damaged or compressed, they become less efficient at sending and receiving signals related to sensations and movement. These nerves also connect to the lower extremities, leading to abnormal sensations in the legs.
Impaired sensory signals can cause numbness, tingling, and “pins and needles” sensations, while damaged or compressed motor nerves can interfere with normal muscle movements. This combination can result in feelings of heaviness in the legs or a sensation that something is pulling or pushing the affected area.
Pain Spreading From Lower Back to Foot
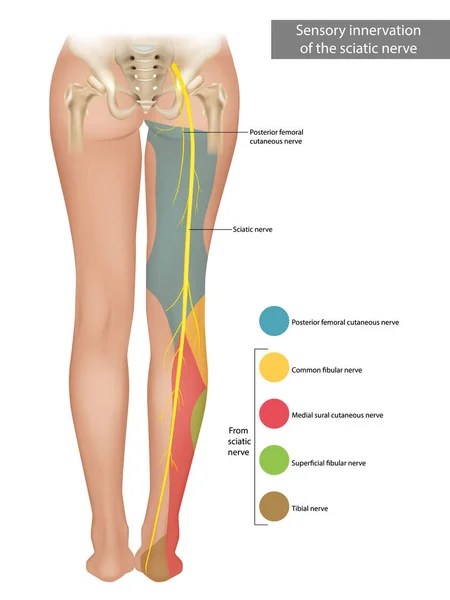
If you have pain that radiates from your pelvis to the lower back, through your leg, and down to your foot, you might have a condition called sciatic endometriosis. This happens when endometrial implants grow on, compress, or cause lesions to the sciatic nerve.
The sciatic nerve is the largest and longest nerve in the body, running from the lower back down the back of each leg. It controls the muscles at the back of the leg and provides sensation to parts of the leg and foot.
When this nerve is compressed or damaged, it can misfire, causing sharp or stabbing pain. It can also lead to numbness, cramps, and spasms.
Pain Occurring On One Or Both Sides
If the endometrial implants affect only the nerves on one side of the body, you might experience pain in just one leg. This can happen if the sciatic nerve is affected or if the abnormal endometrial growths impact the obturator nerve, which controls the movement of the thigh.
However, studies show that nearly 60% of women with endometriosis-related leg pain feel pain and numbness in both legs.
This detail is important in figuring out what’s causing your pain. For instance, in people with leg pain caused by sciatica, symptoms usually appear in one leg because only one sciatic nerve is affected. If both legs hurt at the same time, endometrial growth might be the cause.
Pain That Intensifies With Menstrual Periods
You can tell if your leg pain is due to endometriosis or if it gets worse with menstruation. During each menstrual cycle, the endometrial implants grow and thicken, leading to more inflammation and lesions.
During menstruation, your body triggers reactions to shed the unneeded endometrium, including cramping. These reactions can intensify the pain you feel and increase the inflammation caused by endometrial implants outside the uterus.
Where In Your Legs Is The Pain Most Intense?
Depending on which nerves are damaged or compressed by endometriosis, you might feel nerve pain in different parts of your lower body.
The nerves most commonly affected by endometriosis due to their location include:
- Sciatic nerve: This nerve signals parts of the thigh, leg, and foot.
- Obturator nerve: This nerve controls the thigh muscles and helps with movements like adduction. If it’s damaged, you might feel pain in the groin and inner thigh.
- Femoral nerve: This nerve starts near the groin and is the main nerve in the thigh.
- Pudendal nerve: This nerve runs through the perineum and buttocks, controlling the genital area. If affected, it can cause pain in the vagina, urethra, and rectum.
Common areas of pain include:
- Outside of the legs: Pain in the outer part of the knees or the outer area of the lower leg and foot happens when the common peroneal nerve, a branch of the sciatic nerve, is affected.
- Back of thighs and calves: Pain in these areas occurs when the tibial and medial plantar nerves, branches of the sciatic nerves, are affected.
- Knees: Knee pain can occur when the tibial or common peroneal nerves are damaged.
Home Remedies To Ease The Pain
Certain risk factors for leg pain related to endometriosis, such as height and age, cannot be changed. However, other factors, like weight gain, stress levels, and lifestyle, can be modified with the right interventions.
Additionally, some self-care strategies, home remedies, and medications may help relieve your symptoms. Since these treatments won’t cure endometriosis and might cause side effects, it is always best to consult a specialized healthcare professional.
Let’s explore some ways to address your symptoms.
Heat Or Cold Packs
Heat packs, such as heating pads and hot water bottles, can help relieve pain by relaxing muscles, easing tension, and reducing cramping. Ice packs applied to your legs or buttocks can reduce blood flow to the affected area, which helps decrease inflammation, swelling, and stiffness.
Try both strategies to see what works best for you. Always protect your skin from extreme heat or cold by wrapping the packs in a protective cloth.
Massage
Massage therapies and alternative treatments like acupuncture may help relieve pain by easing muscle tension, improving blood circulation around the affected area, and promoting relaxation and well-being.
While massage therapy can benefit some people with endometriosis, results vary from person to person and may not last after the treatment stops.
Oral Medications
If self-care strategies and home remedies don’t work, certain oral medications can help. Commonly prescribed treatments for endometriosis pain include:
- NSAIDs: Non-steroidal anti-inflammatory medications, like ibuprofen, can temporarily relieve pain and discomfort associated with inflammation.
- Hormonal Therapies: Hormonal treatments, such as birth control pills, may reduce the production of hormones that control ovulation and menstruation, preventing endometrial implants from thickening during your menstrual cycle and alleviating pain.
- Muscle Relaxers: These medications can reduce spasms and cramps, relieving pressure on surrounding nerves and helping to alleviate pain and discomfort.
Other options include vaginal valium, therapeutic injections, and anticonvulsants. If other treatments don’t work or if leg pain disrupts daily life, laparoscopic surgery to remove abnormal endometrial tissue may be recommended.
Nerve Blocks
Nerve block treatments are a valuable option for managing the chronic pain associated with endometriosis. By injecting medication around specific nerves, these treatments can interrupt pain signals sent to the brain, providing significant relief. For individuals with endometriosis, nerve blocks can target the nerves responsible for pelvic pain, offering a focused approach to pain management.
Nerve blocks for treating endometriosis pain include blocking the previously mentioned nerves that can be commonly affected, including the sciatic, obturator, femoral, and pudendal.
If these fail, laparoscopic surgery to remove endometrial tissue may be recommended for severe leg pain.
When Should You Consult A Doctor
With endometriosis, the pain you feel doesn’t always match the severity of your condition. You might have extensive endometrial implants and no pain, or mild endometrial growths that cause intense discomfort. Because of this, it’s crucial to talk to a doctor as soon as you notice any symptoms that might be related to endometriosis.
In particular, you should seek medical care if:
- The leg pain develops suddenly and becomes severe
- At-home remedies are ineffective and your pain is getting worse
- The leg pain is accompanied by other symptoms, such as excessive bleeding, blood in the urine, and pelvic pain
- The pain has started to interfere with your daily life and mental health
It’s important to remember that if endometrial implants damage or irritate nerves, they can cause permanent lesions and damage. This can lead to severe or chronic neuropathy (nerve pain), which might continue even after treatments have removed the abnormal endometrial growths. Studies show that around half of people with endometriosis exhibit signs of neuropathic pain and nerve damage.
Diagnosing Endometriosis-Related Leg Pain
Leg pain caused by endometriosis is very hard to diagnose, especially when no other symptoms are present. If you suspect endometriosis, your doctor may perform several diagnostic tests to rule out other causes of leg pain, such as peripheral artery disease, or deep vein thrombosis (DVT).
Some diagnostic tools your doctor may use include:
- A review of your medical history
- A survey about your symptoms, including their nature, intensity, and location (e.g., if the leg pain worsens during menstruation)
- A thorough physical examination
- A pelvic exam
- Imaging and ultrasound tests, like CT scans, MRI scans, or transvaginal ultrasounds (these are recommended if a pelvic exam suggests endometriosis is causing the leg pain)
- Surgeries like laparoscopy, which allow the surgeon to see and remove endometrial implants
Certain tests for neuropathy, such as skin biopsies, nerve conduction tests, and electromyograms, may also be used. These tests help determine the number of nerve fibers under the skin and their ability to send and receive signals. Neurological tests may also be prescribed.
Discover Relief From Leg Pain Caused by Endometriosis
Endometriosis can be treated with a comprehensive approach to pain management.