Rheumatoid arthritis (RA) affects over 1.3 million people in the US, making it a leading cause of chronic pain and disability. Within two to three years of diagnosis, 30% of patients become work-disabled, while 41% experience activity limitations and 11% face social restrictions.
Since there is no cure, treatment focuses on symptom management through medications, therapies, and sometimes surgery. This ongoing struggle leads to depression in nearly 48% of patients.
At NextPain Care, we focus on improving the lives of those with RA. Our advanced treatments are designed to enhance your overall health and well-being. With our support, you can look forward to a better quality of life despite an RA diagnosis.
What Is Rheumatoid Arthritis?
RA is a type of inflammatory arthritis, an autoimmune disease that occurs when the body’s immune system mistakenly attacks healthy tissues. This lifelong condition causes pain and stiffness in several joints across the body and, if left untreated, can lead to permanent joint damage and disability.
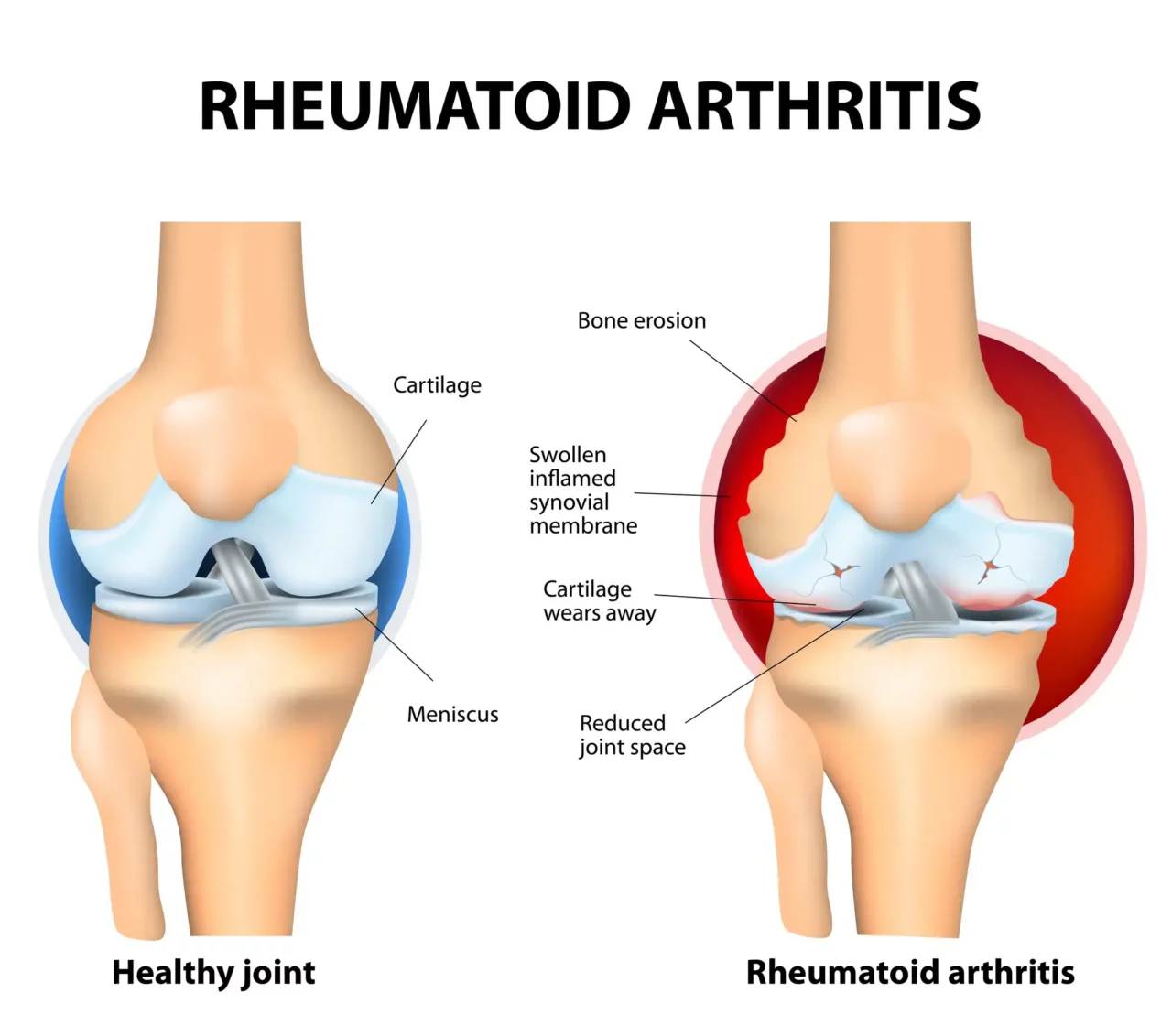
To better understand what RA is and how it develops, let’s start by looking at how healthy joints work. Synovial joints, such as those in the knees, hips, and shoulders, have key features:
- Ligaments and tendons: Connect bones to muscles, regulating movement and preventing injuries.
- Articular cartilage: A cushion at the ends of bones that allows smooth, frictionless movement.
- Synovium: A thin membrane that produces fluid to lubricate and protect the joint.
- Tenosynovium: A lining within tendon tunnels that reduces friction and enables smooth tendon gliding.
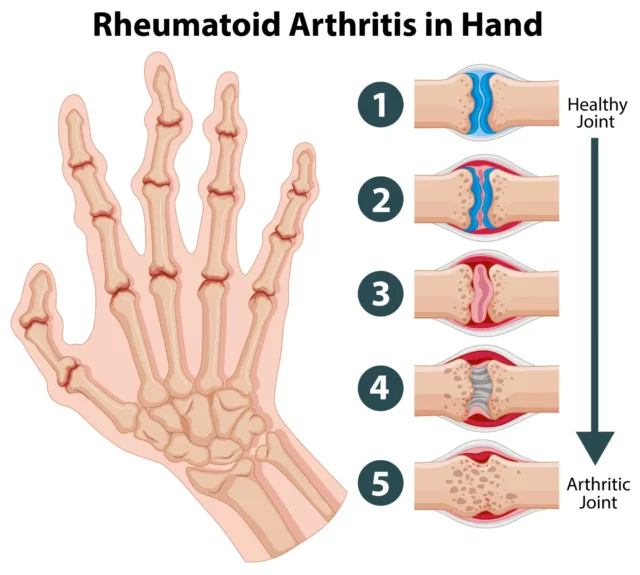
RA occurs when immune cells mistakenly attack healthy tissues, particularly the synovium and tenosynovium. This triggers inflammation, causing the synovium to swell and thicken, eventually spreading to cartilage and bones. When the tenosynovium is inflamed, the surrounding tendon sheaths can swell, leading to tendodn damage and tears.
However, thanks to advanced treatment options, it is now possible to modify the disease, prevent the progression of joint damage, and avoid the most serious complications of RA, including deformities and joint destruction.
Understanding The Symptoms Of Rheumatoid Arthritis
The symptoms of rheumatoid arthritis vary greatly, depending on how advanced the disease is and which joints are affected. However, most people with this condition report the following symptoms:
- Pain around and radiating from the affected joint
- Joints that ache even when at rest
- Joint swelling, redness, and warmth, resulting from inflammation
- Stiffness, especially after periods of rest (in the mornings or after sitting for a long time)
- Symptoms that spread across the body, such as fever, low energy levels, and loss of appetite
- Complications of inflammation, including dry eyes and chest pain
- Fatigue and weakness, often due to low levels of red blood cells (anemia)
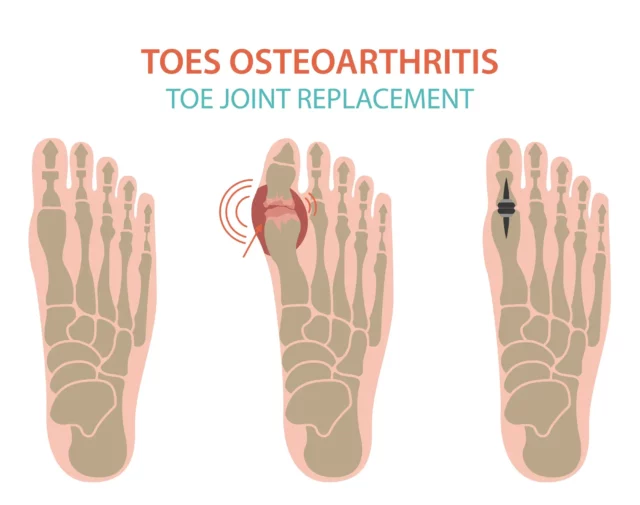
- Deformities and contractures (the stiffening and shortening of tissues in the joint), such as bunions and hammer toes
- Nodules or fleshy lumps—known as rheumatoid nodules—present in up to 25% of people with RA.
The joints most commonly affected by RA are fingers, hands, wrists, knees, ankles, feet, and toes. The early symptoms of RA are usually felt in the smallest joints of the fingers and toes, typically affecting the same joint on both sides of the body (e.g., both hands or both feet).
As the condition progresses, pain, swelling, and stiffness become more intense, especially during flare-ups. Even in remission, unchecked inflammation can lead to joint damage, weakness, and disability, making consistent care essential.
Crepitus Explained: What You Need to Know
Crepitus, the term describing the grating sensation in joints, often signals an underlying issue of greater concern. This sensation manifests as crunching, cracking, or popping sounds and feelings during joint movement, potentially linked to conditions such...
Joint Pain And Swelling
Joint pain is undeniably prevalent across all adult age groups and ranks among the most common musculoskeletal issues. However, its ubiquity does not diminish its impact; joint pain and swelling can severely restrict mobility, causing stiffness, throbbing...
Muscle Spasm In The Stomach
Experiencing a muscle cramp can be painful and uncomfortable. While cramps can occur in any area of the body, muscle spasms in the stomach are particularly common. In fact, almost everybody will experience muscle spasms of some kind throughout their lifetime....
Joint Sensations Of Heat Or Warm
A warm joint happens when there is an increase in joint temperature above normal levels. This sensation can manifest as heat emanating from the joint, often accompanied by swelling, redness, and discomfort. If you're also experiencing symptoms like fever or...
Patellar Tendon Pain
The patellar tendon is a strong band of tissue responsible for keeping the kneecap in place, stabilizing the knee, and enabling movements like jumping, running, and squatting. Despite how reliable and resilient this tendon is, overuse and age-related tissue...
Jaw Immobility
When opening the mouth, the lower jaw normally moves away from the temporal bone of the skull. However, when this natural movement is hindered by pain or discomfort, it results in a condition known as jaw locking. This condition can severely impact one's...
Factors That Lead To The Development Of RA
The exact cause of RA is unknown. However, researchers have shown that certain environmental factors may act as triggers, which activate the disease in people who carry certain genes. Even though RA isn’t considered an inherited disease, when the body is exposed to these triggers, the immune system begins to respond incorrectly, leading to rheumatoid arthritis.
There are several known triggers for RA, and they may vary from one person to another. However, the most common ones include:
- Genetics: Certain genes, like HLA, increase the risk of RA, especially when combined with triggers such as smoking or poor diet. Having a family history of RA further raises susceptibility.
- Hormones: Hormonal imbalances, particularly in estrogen and progesterone, are linked to a higher risk of RA. This helps explain why women are more prone to RA than men.
- Infection: Viral infections like Epstein-Barr can overstimulate the immune system, triggering chronic inflammation that may lead to RA, especially in those with strong immune responses.
- Smoking: Smoking is a key RA trigger that worsens symptoms and reduces medication effectiveness. Even after quitting, former smokers remain at higher risk.
- Stress: Chronic physical or emotional stress can increase inflammatory responses, making RA more likely. Effective stress management can help reduce this risk.
- Other triggers: Factors like trauma, pollutants, obesity, inactivity, poor sleep, and extreme weather can disrupt the immune system and contribute to inflammation.
There are also other known triggers to RA, including trauma, pollutants, obesity, medication issues, overexertion, sleep problems, being physically inactive, and even certain weather events. While there’s a lot yet to be understood about the link between these trigger factors and RA, most of them affect the body’s immune response and systemic inflammation in one way or another.f
Who Is At Risk For RA?
Since the cause of RA isn’t well understood, it can be challenging to identify who is likely to be at greater risk of this disease. However, there are some known risk factors worth being aware of. These include:
- Age: RA can affect anyone, at any age. However, diagnosis is more common between the ages of 30 and 60. Younger people, especially children and adolescents, may also develop a form of RA known as juvenile idiopathic arthritis (JIA), which differs in several ways from rheumatoid arthritis in adults.
Three-quarters of people with arthritis are within their working age when they are first diagnosed. - Gender: Women are two to three times more likely to develop RA due to hormonal differences and a typically stronger immune response, making them more prone to autoimmune conditions.
- Heredity: While RA isn’t directly inherited, having a first-degree relative with RA increases the risk five-fold, indicating a strong genetic component.
- Weight: Excess body fat increases inflammation through cytokine production, making obese individuals more susceptible to RA and reducing medication effectiveness.
- Joint injury: Fractures or dislocations can trigger chronic inflammation in the affected joint, potentially leading to the onset of RA over time.
- Infection: Inflammatory responses triggered by infections, such as viral or bacterial illnesses, can become uncontrolled and increase the risk of RA development.
These risk factors tend to act as triggers in individuals with a predisposition toward rheumatoid arthritis. For example, testing positive for certain markers, such as rheumatoid factor (an antibody commonly found in RA patients) or antinuclear antibodies (which are associated with various autoimmune conditions), could indicate an increased likelihood of developing RA. We’ll look into these aspects later in this guide.
Possible Complications of RA When Left Untreated
As we have seen, the latest advancements in research are helping patients avoid the most severe complications of RA and prevent disease progression. Nonetheless, if left unaddressed, the uncontrolled inflammation that fuels rheumatoid arthritis can lead to a range of severe complications.
Below, we’ll look at the most common conditions that occur when RA—and its underlying systemic inflammation—are left untreated.
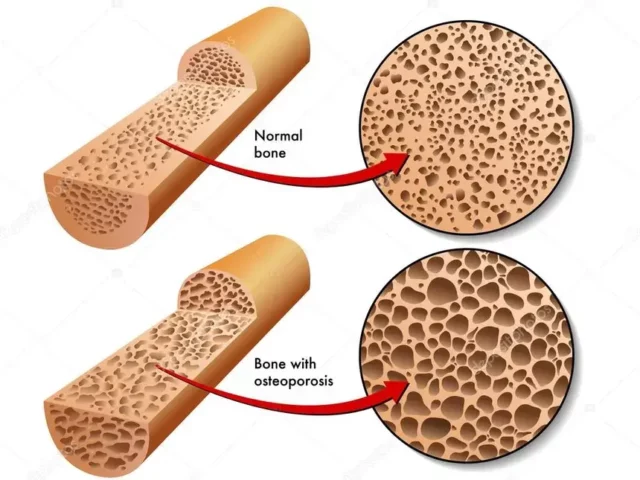
Osteoporosis
Osteoporosis, marked by brittle, porous bones, often remains “invisible” until fractures occur, leading to significant pain. These fractures commonly affect the hip, wrist, or spine, causing sharp or chronic pain that can severely limit mobility.
In people with RA, especially if untreated, chronic inflammation accelerates bone loss and erosion, making bones more prone to fractures and increasing pain in affected areas. Large cysts that form near inflamed joints further contribute to discomfort. Studies show that nearly 30% of RA patients have low bone density or osteoporosis, compounding their overall pain and reducing their quality of life.
Rheumatoid Nodules
Rheumatoid nodules are firm lumps that form near joints affected by RA. While typically painless, they can cause pain or discomfort when they grow large enough to press on nearby nerves. These nodules commonly develop on the elbows, fingers, and knuckles but can appear near any inflamed joint.
Their formation is linked to high inflammation levels and disease progression, especially in people with long-term RA or high rheumatoid factor levels. Smoking and certain medications, like methotrexate, can increase the likelihood of nodules. Although historically seen in 30% of RA patients, effective inflammation control can help prevent painful nodules.
Sjogren’s Syndrome
Sjogren’s syndrome is an autoimmune disorder where the immune system attacks moisture-producing glands, leading to dry eyes and mouth. This can irritate, burning, and sensitivity that may lead to pain in the eyes and difficulty swallowing. Joint pain and fatigue are also common symptoms.
People with RA have a significantly higher risk of developing Sjogren’s syndrome, with up to 31% of RA patients showing signs of the condition. The underlying immune dysfunction in RA often paves the way for other autoimmune disorders, amplifying joint pain and contributing to widespread discomfort and fatigue.
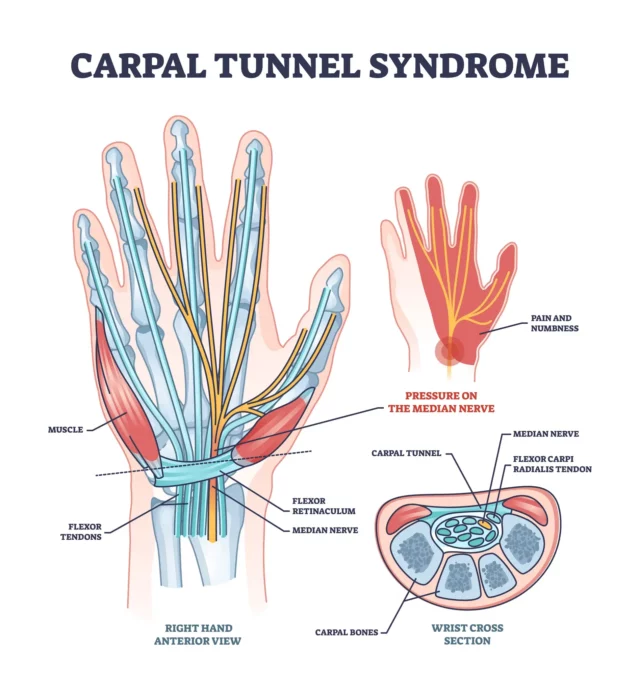
Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) is a condition where the median nerve in the wrist becomes compressed, leading to pain, numbness, and tingling in the hand and fingers (excluding the little finger). This can cause weakness and difficulty with hand movements, impacting daily tasks.
RA increases the risk of carpal tunnel syndrome due to inflammation in the synovium and tenosynovium, causing fluid buildup that narrows the carpal tunnel. This swelling can place additional pressure on the nerve, leading to significant discomfort. Studies show that up to one-third of RA patients may develop carpal tunnel syndrome, making it a common RA-related complication.
Heart Problems
Heart problems linked to RA often stem from chronic inflammation affecting the heart and blood vessels. This can lead to atherosclerosis, where arteries narrow and harden, causing chest pain or discomfort (angina) that may spread to the shoulders, arms, or jaw.
In some cases, inflammation around the heart (pericarditis) results in sharp chest pain that intensifies with breathing or certain movements. People with RA have a 50-70% higher risk of cardiovascular issues, making heart-related pain a common complication.
Lung Disease
RA can cause lung inflammation and scarring (fibrosis), leading to breathing difficulties and chest pain. Conditions like interstitial lung disease (ILD) and pleuritis can cause sharp, stabbing pain during deep breaths or coughing. The chronic inflammation can also weaken respiratory muscles, leading to muscle soreness and chest wall discomfort.
Over time, this combination of lung complications and reduced respiratory capacity can lead to persistent shortness of breath, fatigue, and discomfort. Studies show that nearly 5% of older RA patients develop significant rheumatoid lung disease, with symptoms ranging from mild tightness to chronic pain and respiratory distress.
Lymphoma
Chronic immune activation in RA increases the risk of developing lymphoma, a type of cancer that originates in the lymphatic system. This condition often presents as swollen lymph nodes, especially in the neck, armpits, or groin, which can become tender and painful as they grow. In some cases, lymphoma can spread to the bone marrow, causing deep, aching bone pain and joint discomfort.
RA patients are twice as likely to develop lymphoma compared to the general population, due to the prolonged inflammatory process that damages healthy immune cells and tissues.
How Is RA Diagnosed?
There is no specific diagnostic test to definitively prove you have RA. What’s more, the early symptoms of RA overlap with those of other conditions, often leading to patients waiting nearly 17 months before initiating treatment.
Nonetheless, your doctor may use a range of examinations and laboratory tests to determine the source of your pain. If RA is suspected, you may be referred to a rheumatologist to confirm the diagnosis. Below, we’ll look at the most commonly used tests in more detail.
- Medical history: Since RA develops gradually, early diagnosis can be challenging. Your doctor will review your family history of RA or autoimmune conditions, overall health, medications, and reported symptoms to identify patterns linked to RA.
- Physical examination: The doctor will palpate your joints to check for tenderness, swelling, limited range of motion, or early deformities. Signs like inflamed tendon sheaths or joint stiffness may indicate RA. In severe cases, they may assess for tendon tears or ruptures.
- Laboratory tests: Although it isn’t possible to diagnose RA using a single test, the following examinations can be extremely helpful when analyzed together. These tests include:
- Rheumatoid factor (RF): Detects RF protein, present in 60-80% of RA patients. However, 40% of early RA cases may not show RF, indicating seronegative RA.
- Anti-cyclic citrullinated peptide (anti-CCP) antibody: Confirms RA presence after the RF test by detecting anti-CCP antibodies. It is more specific to RA, and a positive result strongly indicates the disease.
- Complete blood count (CBC): Analyzes red and white blood cells and platelets to detect inflammation-related anemia or abnormal immune responses.
- Erythrocyte sedimentation rate (ESR): Measures how quickly red blood cells settle in a test tube. A faster rate indicates higher inflammation levels.
- C-reactive protein (CRP): A protein produced by the liver in response to inflammation. Elevated levels indicate significant inflammation and help monitor treatment effectiveness.
- Imaging tests: Imaging tests provide a clear picture of the inner aspects of your joints, allowing your doctor to determine the presence of inflammation, abnormalities, and, in the case of RA, the extent of damage. Different tests can examine different types of tissues. These include:
- X-ray: Shows bone damage, joint space narrowing, and erosions but may not detect early RA changes.
- CT scan: Provides detailed cross-sectional images to detect bone damage not visible on X-rays.
- MRI: Creates high-resolution images to reveal early inflammation and joint damage.
- PET scan: Tracks radioactive tracers to detect inflammation sites and evaluate tissue activity.
- DEXA scan: Measures bone density, identifying early signs of osteoporosis related to RA.
These tests, alongside ultrasound scans and more specific laboratory tests, can be used as stand-alone diagnostic tools or in combination with other methods to determine the presence of RA.
Common Treatment Options For RA
As mentioned, there is no permanent cure for RA. However, several treatment plans can help you manage your symptoms and modify the disease. The most common goals for treatment for RA include:
- Easing symptoms
- Putting the disease into remission by stopping inflammation or reducing it to the lowest possible level
- Preventing permanent damage to joints and surrounding organs
- Preventing long-term complications
To achieve these goals, your doctor may use medications, conservative treatments, and surgical interventions to reduce inflammation as quickly as possible, monitor inflammation levels, and work toward low or no symptoms.
You may also be recommended lifestyle modifications that can help lower inflammation and manage symptoms. These include changing your diet, losing excess weight, incorporating movement into your daily routine, and focusing on quality sleep and stress management.
In the sections below, we’ll explore the traditional treatments prescribed for RA, along with their benefits and limitations.
Medication
Medications are often the first port of call for patients with RA. There are several types of medications that may help with this condition, subdivided into two categories:
- Medications that don’t modify the disease but relieve its symptoms. These include painkillers, non-steroidal anti-inflammatory drugs (NSAIDs), and corticosteroids.
- Medications that modify the course of the disease. These include disease-modifying anti-rheumatic drugs (DMARDs), which can be biologic or nonbiologic and are managed by a rheumatologist.
These medications are often used in combination to tackle multiple aspects of the disease. Moreover, when complications of RA occur, these comorbidities may also need to be addressed. As a result, many patients follow a complex medication regimen involving more than one medication. Below, we’ll look in more detail at treatment options available today:
Painkillers: Over-the-counter options like ibuprofen help manage flare-up symptoms but do not modify the disease.
Corticosteroids: Short-term use reduces inflammation and pain until long-term medications take effect.
NSAIDs: Block COX enzymes to reduce pain and inflammation.
DMARDs: Slow disease progression by suppressing the immune system. These include:
- Nonbiologic DMARDs (e.g., methotrexate) suppress the immune system broadly but may take months to work.
- Biologic DMARDs target specific inflammatory cells for faster results.
- JAK inhibitors block signals that trigger inflammatory cell production, helping to control symptoms.
Heat And Cold
One popular at-home care strategy for rheumatoid arthritis relief is using an ice pack or hot compress. These work in different ways, and you may find that one works better for your specific needs.
- Cold therapy: Ice constricts blood vessels, reducing inflammation and swelling. This helps temporarily relieve joint pain and stiffness, improving mobility.
- Heat therapy: Heat increases blood flow and oxygen around the joint, relaxing muscles, easing nerve pressure, and providing a sense of relief.
While this method doesn’t treat RA itself, it can help manage pain during flare-ups. For the best results, heat and cold therapy should be combined with medications or physical therapy.
Joint Immobilization
Joint immobilization involves using braces or splints to restrict movement, stabilize joints, and prevent further damage. This technique reduces joint stress during physical activity. However, prolonged use can lead to stiffness, muscle weakness, and atrophy, so it’s essential to follow your rheumatologist’s instructions.
Massage
Massage therapy helps reduce muscle tension, relieve nerve pressure, and ease joint pain, improving mobility. Techniques such as Swedish massage have been shown to be effective in reducing discomfort and the need for pain medications. It’s important to choose a therapist experienced in RA treatments to avoid exacerbating your symptoms.
Acupuncture
Acupuncture is known to trigger the release of endorphins and reduce inflammation, improving pain levels and overall well-being. Research shows it can enhance mobility and reduce RA symptoms without significant side effects. However, it may not be suitable for those with bleeding disorders or who take blood thinners.
Surgery
If RA isn’t responding well to conservative treatments or has caused permanent joint damage and disability, your doctor may recommend surgery. Different orthopedic surgical interventions may help reduce RA complications. These include:
- Synovectomy: Removes inflamed synovial tissue to ease pain in early RA stages but doesn’t stop the disease from affecting other joint components.
- Tendon repairs: Repairs torn or ruptured tendons, strengthens weak areas, and releases tight tendon sheaths to restore mobility.
- Joint rebalancing: Corrects deformities and contractures, improving joint alignment and function, and reducing pain.
- Joint replacement (arthroplasty): Replaces damaged joint components with artificial parts, restoring movement and function.
- Joint fusion: Fuses two bones into one by reshaping bone ends. This eliminates pain but restricts movement and is typically used for small joints.
No matter the type of surgery, understanding the full process is important. Rehabilitation is a key part of recovery and includes managing healing and monitoring for complications. While surgery can help reduce pain and slow RA progression, it works best as part of a broader treatment plan. Consulting with an orthopedic specialist or rheumatologist can provide a clear view of the potential benefits and considerations.
The NextPain Care Approach To Treating Rheumatoid Arthritis
Physical Therapy
Physical therapy is a crucial component of pain management that involves exercises and techniques to improve movement and reduce pain. NextPain Care offers personalized physical therapy programs to help patients regain strength, flexibility, and function...
Joint Injections
Joint injections are used to deliver medication directly into a joint to reduce inflammation and pain. At NextPain Care, these injections, which can include steroids or synthetic joint fluid, provide a minimally invasive option for managing arthritis and...
Radiofrequency Ablation
Radiofrequency ablation is a procedure that uses heat to disable nerves responsible for transmitting pain signals. At NextPain Care, this minimally invasive treatment is utilized to address chronic pain conditions, particularly in the spine. NextPain Care's...
"Treatment options are tailored to your individual needs, and availability may vary based on factors such as location and insurance. We’re here to guide you through the possibilities and help determine the best course of action for your journey to relief and recovery."
Start Your Journey To Better RA Management Today
Our Providers
We take great pride in the wealth of talent and expertise that our providers have as they improve the health outcomes of our patients, each and every day.
Modalities Associated with Rheumatoid Arthritis

Mindfulness and Meditation for Chronic Pain
Mindfulness and meditation are techniques used to manage chronic pain by promoting relaxation and mental focus. NextPain Care incorporates these practices into its holistic approach to pain management, helping patients reduce pain perception and improve their...

Physical Therapy
Physical therapy is a crucial component of pain management that involves exercises and techniques to improve movement and reduce pain. NextPain Care offers personalized physical therapy programs to help patients regain strength, flexibility, and function...
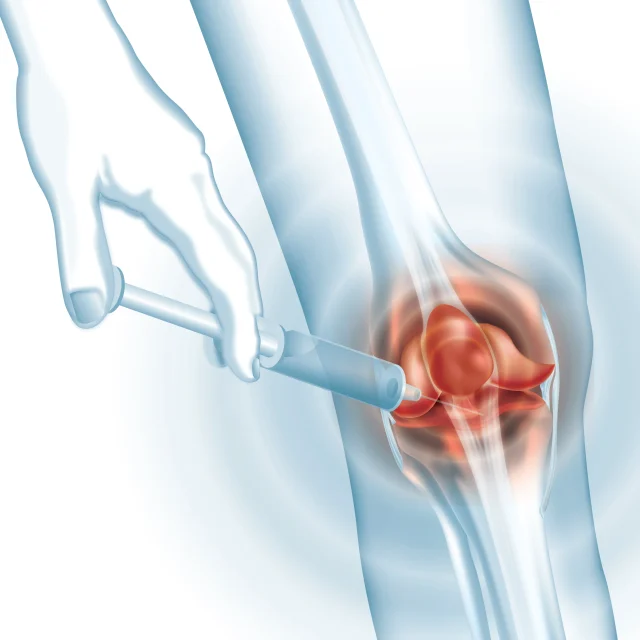
Joint Injections
Joint injections are used to deliver medication directly into a joint to reduce inflammation and pain. At NextPain Care, these injections, which can include steroids or synthetic joint fluid, provide a minimally invasive option for managing arthritis and...

Radiofrequency Ablation
Radiofrequency ablation is a procedure that uses heat to disable nerves responsible for transmitting pain signals. At NextPain Care, this minimally invasive treatment is utilized to address chronic pain conditions, particularly in the spine. NextPain Care's...
Don't let pain and discomfort hold you back any longer.