Interstitial cystitis (IC) is a long-lasting condition that affects the bladder, leading to continuous pain and discomfort in the lower abdomen. Beyond the pain, various other unpleasant symptoms can develop throughout the urinary system, significantly disturbing different parts of a person’s daily life. These disturbances can affect work, mental health, and relationships, having a large impact on daily living.
This guide aims to shed light on the complex nature of IC, exploring its causes, symptoms, diagnostic methods, and the potential impacts on those diagnosed with this chronic pain condition. We will also discuss both medical and complementary treatment options commonly used to alleviate IC discomforts.
Our goal is to help you understand the source of your discomfort, make informed health decisions, and find the best approach to managing your IC pain, thereby improving your quality of life and helping you regain a sense of normalcy.
Let’s begin by taking a closer look at the anatomy of the bladder and exploring the pathophysiology of IC.
Exploring the Anatomy of the Bladder
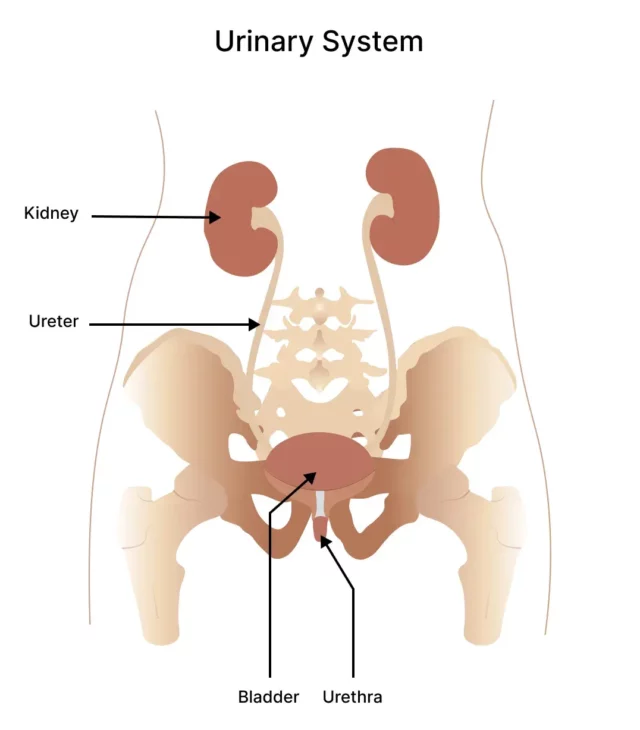
The urinary system is one of the most complex networks in your body, consisting of four main parts: the kidneys, ureters, bladder, and urethra. This network of organs plays a crucial role in maintaining overall health by regulating various essential processes in the body. Let’s delve a little deeper into this system.
It starts with the kidneys, two vital organs responsible for filtering waste products and excess fluids from the bloodstream. Within their bean-like structure are complex filters that sift the blood to remove toxins and excess fluids. This filtered fluid becomes urine, which is delivered from the kidneys to the bladder through two slender tubes called ureters.
The bladder sits at the core of the urinary system, responsible for storing and releasing urine. Located in the lower abdomen, this pear-shaped, muscular, hollow sac is connected to an extensive network of nerves. These nerves play a crucial role by sending messages to the brain, signaling when the bladder is full and prompting the need for urination.
Functioning as a reservoir, the bladder gradually expands to hold approximately 400-600 milliliters of urine. When full, nerve functions prompt the bladder to contract and smoothly release urine through the urethra, exiting the body in the process of urination. After this, nerve activity decreases, allowing the bladder to relax and prepare for the next cycle.
Any disruptions to this system, like those seen in conditions such as IC, can affect its delicate balance. Next, we’ll discuss what specifically affects the urinary system and causes the pain and uncomfortable symptoms associated with IC.
What Is Interstitial Cystitis (IC)?
IC is a long-term pain condition where the bladder wall becomes inflamed and irritated, causing persistent discomfort that lasts for six weeks or more without a clear cause. Also known as “painful bladder syndrome” or “frequency-urgency-dysuria syndrome,” IC affects the complex physiology of the urinary system, especially the bladder and urethra.
Ongoing inflammation in the bladder can cause muscle scarring, leading to stiffening of the bladder wall. Over time, this reduces its ability to expand and contract as it once could, lowering the bladder’s total urine-holding capacity.
Additionally, persistent bladder irritation significantly impacts the nerves around the bladder, disrupting communication with the brain and muscles. This disruption can trigger various distressing symptoms, with pain and pressure being primary features. Let’s take a closer look at these symptoms.
Identifying The Signs of Persistent Bladder Discomfort
Interstitial Cystitis (IC) is a condition that varies greatly among individuals. Symptoms can range from occasional flare-ups to constant challenges. Here are some common difficulties faced by those with IC:
Pain and Discomfort
IC is known for causing persistent pain and discomfort. Symptoms may include a constant ache, increased pressure, or a sharp sensation in the pelvic area, lower abdomen, or perineum (the area between the anus and the scrotum or vulva).
The intensity of the pain can vary, from mild discomfort to severe, incapacitating sensations. Typically, the discomfort worsens as the bladder fills and improves after urination.
Urinary Urgency and Frequency
People with IC often feel a strong need to urinate more frequently than usual, even if the amount of urine is small.
This urgency and frequency occur because the bladder’s irritated nerves send incorrect signals to the brain, indicating it’s time to urinate even when the bladder isn’t full. Alternatively, the bladder might not stretch as much as it should, making it feel full and needing to be emptied more frequently.
Urinary Incontinence
In severe cases, IC may lead to urinary incontinence. This is when individuals have difficulty controlling their bladder, resulting in involuntary urine leakage. This challenging symptom is more common in older adults with IC or during times of urgency or physical exertion.
Urinary incontinence adds another layer of complexity to the daily lives of those dealing with IC, requiring constant awareness and management.
Intimacy Issues
The challenges associated with IC may extend to intimate aspects of life. Pain and discomfort can make sexual activity difficult and, in some cases, extremely painful.
This symptom is believed to stem from spasms in the pelvic floor muscles, which support the bladder, bowel, and either the uterus or prostate. The fear of worsening symptoms during sex may contribute to anxiety and strain relationships.
Understanding the symptoms of IC is the first step in managing its ongoing challenges. This chronic bladder condition can significantly affect a person’s quality of life.
Next, we’ll explore the causes of IC, highlighting some of the factors linked to this condition.
Causes of Chronic Bladder Problems
Experts are still researching to discover the exact cause of IC. However, some theories suggest complex interactions between the immune system, nerves, and the bladder lining. Let’s explore some of these potential triggers in the headings below:
Bladder Inflammation
Inflammation is a key aspect of the pathophysiology of interstitial cystitis. Unlike a urinary tract infection (UTI), IC inflammation doesn’t necessarily result from bacterial infection.
It’s suspected that IC inflammation may be due to damage or dysfunction of the protective mucosal lining of the bladder. This damage leads to urine or other harmful components coming into contact with the delicate lining of the bladder, causing inflammation. This inflammation brings further irritation, pain, and increased sensitivity to the bladder and pelvic region.
Pelvic Floor Dysfunction
Pelvic floor dysfunction is identified as another potential cause of or co-existing condition with interstitial cystitis. The pelvic floor consists of many strong muscles, ligaments, and connective tissues that support the bladder, rectum, and reproductive organs.
Dysfunction of the pelvic floor network, whether excessively tight or too weak, can cause pelvic pain, urinary urgency, and altered bladder function. Addressing pelvic floor issues through physical therapy and targeted exercises is a common approach to managing interstitial cystitis symptoms.
Autoimmune Disorders
There is a strong relationship between a number of autoimmune disorders and interstitial cystitis, suggesting potential immune system involvement in the development of the condition. Autoimmune conditions such as fibromyalgia, irritable bowel syndrome (IBS), and chronic fatigue, among others, have all been associated with an increased risk of interstitial cystitis.
In autoimmune-related IC, the immune system may mistakenly target the bladder’s smooth muscle receptors, leading to inflammation and damage. Understanding these connections can help healthcare professionals tailor treatment approaches for individuals with autoimmune-related IC.
Nerve Damage
Damage to the bladder’s intricate nerves is another potential contributor to interstitial cystitis, affecting communication between the bladder, spinal cord, and brain. When these nerves sustain damage or dysfunction, it can lead to abnormal sensations, heightened pain perception, and disruptions in bladder control.
Nerve damage may have physical causes, such as a spinal cord injury, surgical complications, or trauma. In rare cases, nerve dysfunction in the bladder region may be associated with medical conditions like diabetes, Parkinson’s disease, or multiple sclerosis (MS).
Ultimately, IC is a multifaceted condition with various and possibly interconnected causes. Identifying these potential factors is crucial for early detection and finding personalized management strategies. Now, let’s explore the daily challenges faced by individuals with IC.
The Daily Impact of Chronic Bladder Discomfort
Dealing with Interstitial Cystitis (IC) brings significant challenges due to its intense symptoms, difficulty in diagnosis, unclear causes, and persistent nature. These factors understandably affect a person’s overall well-being, bringing both physical and psychological challenges. Daily challenges for those with IC can include:
Physical Limitations
Physical limitations are sometimes the most significant everyday challenges for people struggling with IC. Chronic pain, ongoing pressure, and urinary symptoms can disrupt daily routines and make even simple tasks uncomfortable.
Additionally, IC symptoms may result in reduced mobility, making regular exercise difficult, as well as complicating participation in social events. Navigating daily life with IC involves understanding and managing these physical limitations.
Emotional and Mental Health
The emotional and mental toll of interstitial cystitis is profound. Dealing with persistent pain, unpredictable symptoms, and the potential for social isolation can contribute to heightened levels of stress, anxiety, and even depression.
The emotional impact is not confined to the individual with IC alone but may also extend to their support network. Relationships, social interactions, and overall involvement in a meaningful life may be affected. Being aware of and addressing the psychological impact of IC is essential for maintaining good emotional and mental health.
Work and Productivity
The physical and psychological impacts of IC can make it tough to stick to regular work routines and stay productive. The need for frequent bathroom breaks, the possibility of pain flaring up, and the mental stress of handling symptoms during work hours can greatly impact a person’s professional life based on how well symptoms are managed. Individuals may need to seek career support to find the right balance for both their work and health needs.
Understanding the broad impact on physical, emotional, and occupational well-being is crucial for individuals with IC, along with their close network of family, friends, and healthcare providers.
By addressing all dimensions affected by IC, individuals have a better chance of navigating its challenges and improving their health outcomes.
Seeking early support from healthcare professionals and exploring various management strategies can contribute to improved quality of life for those living with IC. We’ll explore the clinical processes of diagnosing IC in the following section.
How to Diagnose Interstitial Cystitis
Diagnosing Interstitial Cystitis (IC) involves a detailed approach to understand symptoms while ruling out other potential causes. Since there is no definitive test for IC, healthcare professionals use a combination of medical history, physical exams, and specialized tests to make a comprehensive diagnosis. Here’s what you can expect during the diagnostic process for IC:
- Medical History: Your doctor will start with a thorough review of your medical history and current symptoms. They will ask about the onset, duration, characteristics, and potential triggers or factors that worsen the symptoms. Important details include the type of pain, changes in urinary patterns, and any other related concerns you may have.
- Physical Examination: A thorough physical exam is conducted to check the pelvic area, including the abdomen, pelvic floor muscles, and genitals. The doctor will touch your belly and feel your abdomen for signs of swelling, stiffness, and areas that are tender.
- Specialized Tests: Several tests are used to rule out urinary tract infections and check the urinary system. These include testing urine samples and blood samples. Beyond lab tests, urodynamic studies can evaluate how your bladder functions and identify any abnormalities in its volume capacity and elasticity.Additionally, a cystoscopy may be recommended. In this procedure, a small camera is inserted through the urethra to provide a direct view of the bladder’s interior, helping detect inflammation or other issues.
- Imaging: In some cases, imaging studies such as ultrasound or magnetic resonance imaging (MRI) may be suggested to rule out other potential causes of symptoms and give a detailed view of the bladder and pelvic area. While imaging alone cannot confirm IC, it offers valuable insights for doctors in ruling out other potential causes.
Diagnosing IC often involves teamwork among your primary care physician, nurses, and specialists. Open communication with your healthcare team is crucial if you have any concerns about your symptoms. This helps them reach an accurate diagnosis quickly, allowing you to start treatment strategies that improve your quality of life.
Conventional treatments can involve various medications, which we’ll discuss more in the following section.
Available Medications For Relief
IC, with its intricate nature and individual symptoms, brings about some unique challenges in terms of treatment. While a range of medications is available to reduce symptom discomfort, it’s crucial to understand that IC management often involves a personalized approach, as responses to medications can vary among individuals.
Tricyclic Antidepressants
Tricyclic antidepressants (TCAs) can be beneficial for the pain and pressure sensations of IC. Beyond their primary role in treating depression, TCAs, such as amitriptyline, can positively impact the urinary tract.
These medications may help by relaxing the bladder and modulating pain signals, providing relief to individuals grappling with the persistent discomfort associated with IC. It’s important to note that the use of TCAs for IC is different from its use in depression, with different dosages and effects.
Antihistamines
While antihistamines are commonly known for dealing with allergies, medications like hydroxyzine can also assist in easing specific interstitial cystitis symptoms like frequency and pain.
The idea behind using them is that they block histamine receptors, which helps reduce inflammation in the bladder lining. Various antihistamines, such as Claritin and Benadryl, might be useful for you. It’s about figuring out which one suits you best.
Pain Relievers
For managing IC symptoms, pain relievers can be an option. Your doctor might suggest nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen to help with pain and discomfort. For more severe cases, long-acting analgesics may be prescribed.
It’s important to discuss with your healthcare provider the best treatment plan for you. This conversation helps ensure that you are well-informed about the options available and how they align with your health goals.
In addition to medications, some individuals find that complementary remedies can provide additional benefits for managing IC symptoms. Let’s explore these alternatives next.
Enhancing Care for Interstitial Cystitis with Complementary Treatments
Some complementary treatments are prescribed alongside medical treatments, providing individuals with a well-rounded strategy to tackle the challenges of this condition. These include:
Bladder Training
Bladder training is a useful method to help individuals regain control over their urinary patterns. It involves a structured technique of scheduled bathroom breaks, gradually extending the time between visits.
For those with IC, bladder training focuses on improving bladder capacity and reducing the urgency and frequency of urination. The goal is to establish a more predictable bathroom routine and restore a sense of control over symptoms.
Trigger Point Therapy
Trigger point therapy is a targeted intervention that addresses specific areas of muscle tension associated with IC symptoms. By identifying and releasing trigger points, particularly within the pelvic floor, this therapy aims to alleviate pain and discomfort.
In the context of IC, where pelvic floor dysfunction can contribute to symptoms, trigger point therapy becomes a valuable tool. It seeks to restore muscular balance, offering relief from the intricate web of symptoms linked to the IC experience.
Bladder Instillation
Bladder instillation, also known as a bladder wash or bath, is a treatment that involves introducing therapeutic substances into the bladder. A solution with medications like dimethyl sulfoxide (DMSO) or heparin is introduced into the bladder through a catheter. The goal of bladder instillation is to calm the irritated bladder lining and ease symptoms.
These complementary treatments aim to offer more targeted therapeutic approaches to manage IC in addition to medications.
In the next section, we’ll explore the innovative therapy provided by NextPain Care and how it brings hope to individuals seeking lasting relief from the pain and inflammation caused by IC.
How NextPain Care Approaches Interstitial Cystitis
For those enduring the persistent pain and debilitating symptoms of Interstitial Cystitis (IC), finding relief is essential. NextPain Care offers a holistic approach to managing IC pain.
We start with minimally invasive treatments aimed at effectively addressing your symptoms. If these initial therapies are not sufficient, we are ready to provide advanced interventions to further relieve your discomfort. Our comprehensive treatment plan includes the following therapies:
Mindfulness and Meditation for Chronic Pain
Mindfulness and meditation are techniques used to manage chronic pain by promoting relaxation and mental focus. NextPain Care incorporates these practices into its holistic approach to pain management, helping patients reduce pain perception and improve their...
Nerve Block
Nerve blocks involve the injection of medication to interrupt pain signals from specific nerves. NextPain Care uses nerve blocks to provide targeted pain relief for various conditions, including chronic pain and acute post-surgical pain. This minimally...
Radiofrequency Ablation
Radiofrequency ablation is a procedure that uses heat to disable nerves responsible for transmitting pain signals. At NextPain Care, this minimally invasive treatment is utilized to address chronic pain conditions, particularly in the spine. NextPain Care's...
"Treatment options are tailored to your individual needs, and availability may vary based on factors such as location and insurance. We’re here to guide you through the possibilities and help determine the best course of action for your journey to relief and recovery."
Our Providers
We take great pride in the wealth of talent and expertise that our providers have as they improve the health outcomes of our patients, each and every day.





Manage Your Interstitial Cystitis symptoms effectively with our help.