Is There A Link Between Endometriosis And Leg Pain?
Endometriosis is a chronic inflammatory condition that impacts over 6.5 million women in the US....
Endometriosis is a chronic and often painful condition that affects 6.5 million women in the United States alone. It can lead to a significant loss of productivity, averaging over six hours per week, and deeply impacts both professional and emotional aspects of life.
Despite its prevalence, around 90% of people with endometriosis report being disbelieved or dismissed by loved ones and healthcare professionals. This guide aims to provide accurate information about endometriosis and explore treatment options available through NextPain Care.
Thanks to advances in research, we now have a better understanding of endometriosis and its symptoms. In addition to medications, hormonal therapies, and surgeries, patients now have access to alternative treatment options, such as electroanalgesia.
To understand endometriosis, it’s important to have an overview of the female reproductive system. The uterus, a pear-shaped organ in a woman’s pelvis also known as the womb, is essential for functions such as menstruation, gestation, and labor. It is lined with endometrial tissue, known as the endometrium.
During the luteal phase of the menstrual cycle, the endometrium thickens to prepare the uterus for a fertilized egg. If pregnancy occurs, the endometrium supports fetal growth by supplying oxygen and nutrients and protecting the embryo from microbial invasions. If pregnancy does not occur, the body sheds the endometrium during menstruation, and new endometrial tissue is created in each cycle.
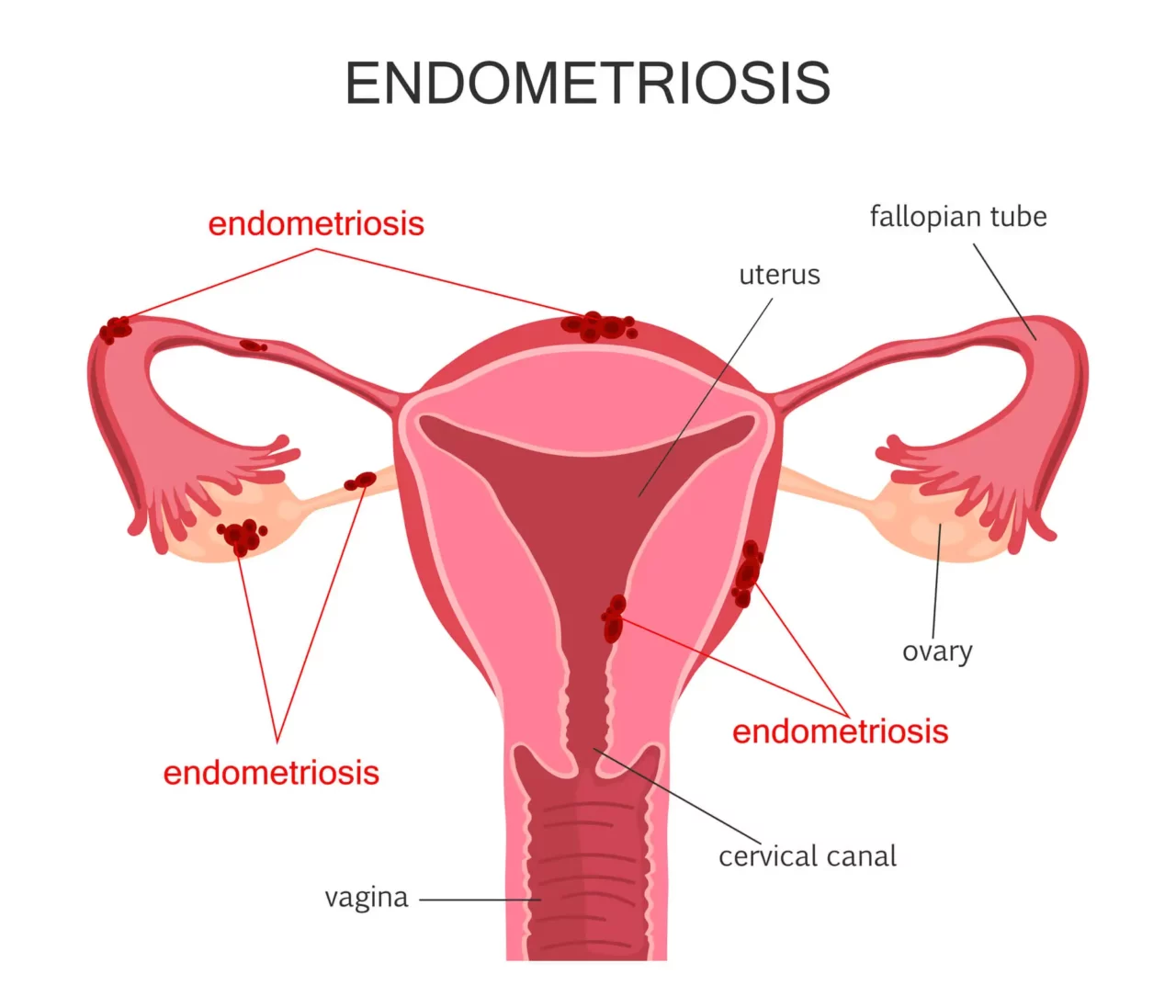
Endometriosis occurs when endometrial tissue begins to grow outside the uterus. These abnormal growths, known as endometrial implants, can affect various organs and tissues around the uterus, including:
In severe cases, endometrial tissue can also be found in the diaphragm and chest.
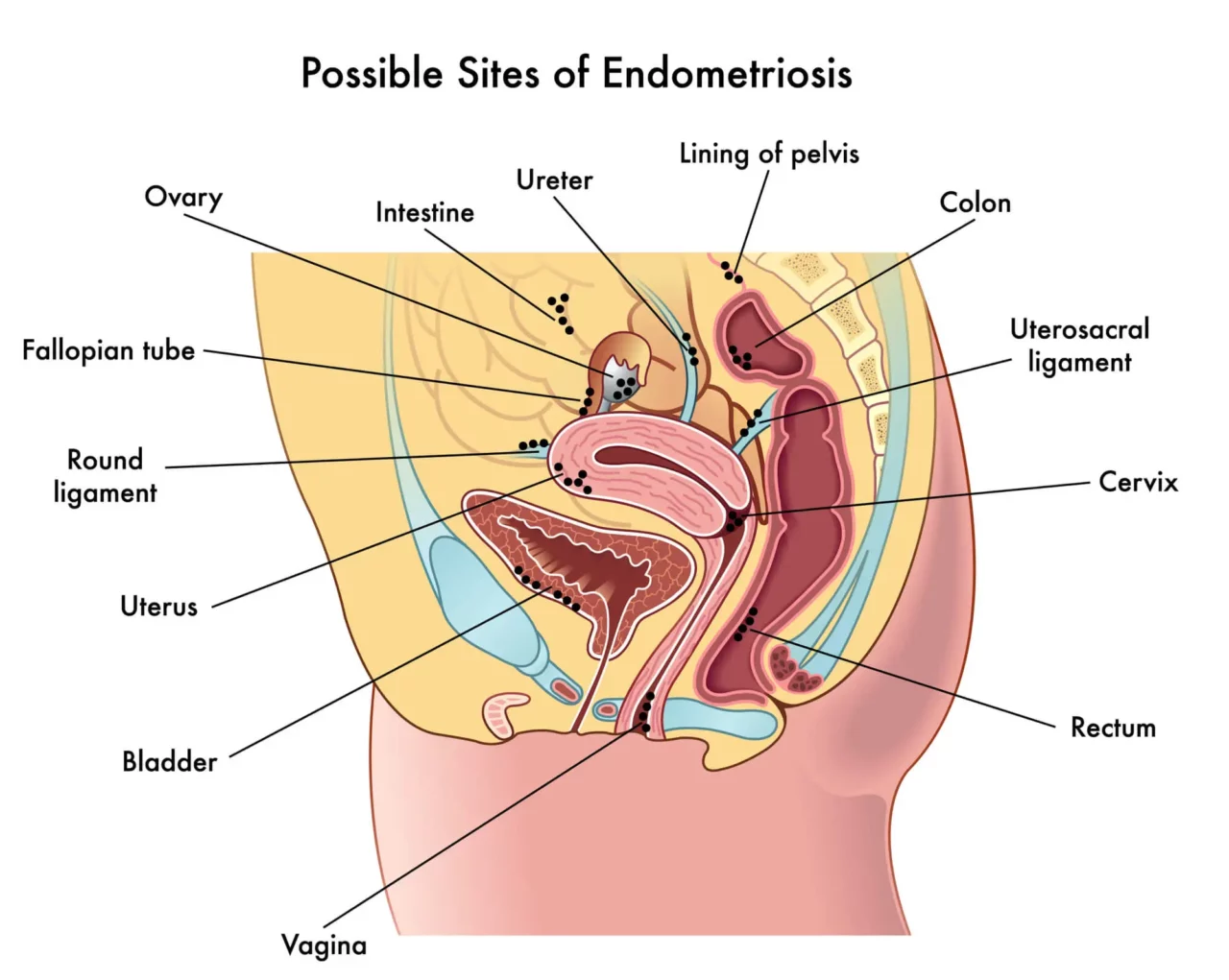
The build-up of abnormal endometrial tissue outside of the uterus can lead to a cascade of complications, including inflammation, scarring, and cysts. The tissue may also bind organs in the pelvis together, causing adhesions and preventing the organs from functioning as they should.
The endometrial tissue that grows outside of the uterus behaves in the same way as the tissue inside the uterus. This means that it responds to the hormonal changes that occur during the menstrual cycle and other events such as menopause.
During your cycle’s luteal phase, the endometrial implants will also grow, swell, and thicken. However, unlike the lining within the uterus, abnormal tissue that grows on other organs cannot easily leave your body during menstruation. This can cause significant pain and other symptoms associated with endometriosis.
Over time, the accumulation of endometrial implants can expand and cause severe problems such as:
Endometriosis is generally classified into stages to describe the extent and location of the abnormal growth of endometrial tissue. It is important to note that the correlation between the spread of endometrial tissue and the severity of symptoms isn’t always straightforward. For instance, some women may experience excruciating pain and severe symptoms even if they have a mild form of endometriosis or are in the early stages of the condition. Conversely, some patients have a severe form of endometriosis and only experience mild discomfort.
Here is a closer look at the stages of endometriosis:
Stage 1 endometriosis is characterized by minimal lesions and small wounds. During this stage, endometrial implants may affect your ovaries and cause inflammation in and around the pelvic cavity.
As the abnormal endometrial growths continue to build up, you may experience stage 2 endometriosis. In this phase, the endometrial implants are still shallow and mostly affect the ovaries and pelvic lining.
Moderate endometriosis causes more and deeper implants, which are usually localized within the ovaries and pelvic linings but may extend to other organs. During this stage, you may also have small adhesions between organs, ovarian cysts, and lesions.
Stage 4 endometriosis is the most severe form of this condition. It involves many deep implants that have spread through the ovaries, pelvic lining, fallopian tubes, and bowels. You may also have large cysts on one or both of your ovaries, as well as severe adhesions between organs.
As we have seen above, the symptoms of endometriosis are not always correlated to the stage of the condition. This means that someone with stage 4 endometriosis might experience very little discomfort, while another person with a mild form might suffer severe symptoms.
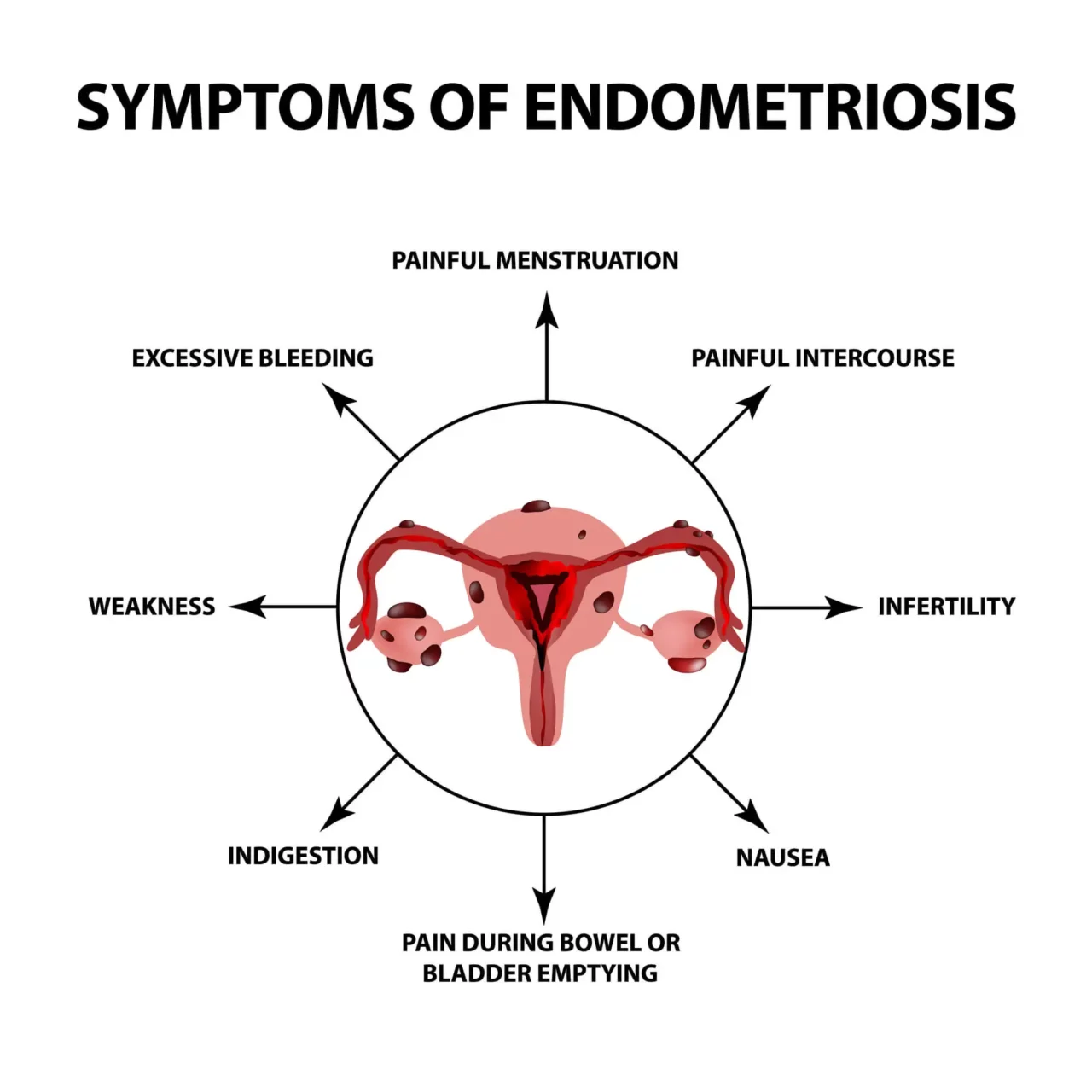
However, only around 20% of women with endometriosis are asymptomatic, often discovering their condition when facing unexplained infertility. The remaining 80% of patients typically deal with chronic pain, painful periods, excessive bleeding, pain during intercourse, difficult bowel movements, digestive issues, and infertility.
These symptoms are often due to endometrial implants outside the uterus that grow, thicken, and bleed during the menstrual cycle but are unable to leave the body during menstruation. This leads to inflammation and irritation of the surrounding tissue.
Additionally, tissue scarring and thickening (fibrosis), as well as adhesions between organs, can contribute to discomfort and pain.
Below, we’ll look at the symptoms of endometriosis in more detail.
One of the most common symptoms of endometriosis is dysmenorrhea, or excessively painful menstrual periods. This condition affects 70-93% of young women and often leads to missed days of work or school. When painful periods are caused by a recognized pelvic condition such as endometriosis, this symptom is referred to as secondary dysmenorrhea.
Endometriosis causes painful periods because the endometrial implants respond to hormonal changes and grow and bleed during the menstrual cycle. Dysmenorrhea manifests itself with several symptoms, including:
Another common symptom of endometriosis is pain during intercourse (dyspareunia), a condition that causes two-thirds of women with endometriosis to suffer from sexual dysfunction.
This symptom occurs because the inflammation of the endometrial growths is aggravated by the thrusting during penetration. In severe cases of endometriosis, pain may also be due to the endometrial implants binding the front wall of the rectum to the back wall of the vagina. These adhesions inhibit the mobility and expansion of the vagina during sex.
Some women with endometriosis experience pain only during deep penetration or have mild discomfort during sex, while others experience sharp and stabbing pain that may last for hours or days after sex. The intensity of pain can vary depending on the stage of the menstrual cycle.
Endometriosis can cause irregular and painful bowel movements. While the connection between these two conditions isn’t entirely clear, the pain is often due to lesions and endometrial growth in the large bowel, bladder, rectum, or intestines.
High levels of sustained inflammation, coupled with the thickening of endometrial growth during the menstrual cycle, make passing stools painful. These painful sensations are often described as stabbing or sharp and are frequently accompanied by other gastrointestinal symptoms such as constipation and bloating.
Endometriosis can alter the frequency and nature of menstruation, leading to excessive bleeding or light bleeding (spotting) between periods. Changes you may experience due to endometriosis include:
These changes occur because people with endometriosis have more blood and endometrial tissue to shed each month.
The connection between endometriosis and infertility is well-documented, though not entirely understood. According to a 2010 study published in the Journal of Assisted Reproduction and Genetics, 25-50% of infertile women have endometriosis, and 30-50% of women with endometriosis are infertile.
Several factors may contribute to infertility in those with endometriosis:
Women with endometriosis can still conceive and carry a pregnancy to term, sometimes with the help of fertility treatments such as in-vitro fertilization (IVF). Additionally, in cases of mild or moderate endometriosis, infertility may only be temporary.
Depending on the location of endometrial growths, those with endometriosis may experience various gastrointestinal problems, known as “endo-belly.” Factors contributing to this condition include:
Endo-belly symptoms include:
A 2022 study indicated that 10-52% of women with endometriosis also suffer from irritable bowel syndrome (IBS).
Fatigue is another common symptom of endometriosis. It becomes more evident during the menstrual cycle when the body attempts to eliminate abnormal or diseased tissue. The immune system releases inflammatory toxins known as cytokines, causing high levels of inflammation and leading to fatigue.
Mild cramps and minor discomfort are common during certain phases of the menstrual cycle. However, up to a third of women experience severe, debilitating menstrual cramps that begin before menstruation and continue after it ends, significantly impacting daily...
Experiencing a muscle cramp can be painful and uncomfortable. While cramps can occur in any area of the body, muscle spasms in the stomach are particularly common. In fact, almost everybody will experience muscle spasms of some kind throughout their lifetime....
Understanding the complex anatomy of the gastrointestinal tract and exploring the negative implications that can come with experiencing painful bowel...
In most cases, stomach pain is nothing more than a temporary, minor issue that resolves itself in a matter of days. However, new surveys have found that 40% of the US adult population - or 60-70 million Americans - struggle with chronic disorders of the...
Dealing with pain during intercourse can be a source of significant distress and discomfort for both partners. In addition to the obvious physical pain, there is often an emotional toll that can be taken when dealing with sexual...
Difficulty conceiving may stem from various factors and could signal an underlying medical condition. Suppose you're experiencing problems conceiving, including dealing with a chronic illness or other health issues. In that case, we hope to provide you with...
A swollen and bloated stomach can result from various causes, including digestive disorders, infections, or food intolerances. It might be accompanied by symptoms such as pain, discomfort, and gas. Persistent or severe bloating should be evaluated by a...
Digestive upset is something many of us encounter occasionally. However, if your digestive issues persist and become more than a temporary inconvenience, they might indicate an underlying...
Endometriosis is considered an idiopathic disease, meaning the exact reasons why endometrial implants and scar tissue grow outside the uterus are unknown. However, since its discovery in the 1860s, several theories have emerged to explain the causes and risk factors of this condition. Some of the most valid hypotheses include retrograde menstruation, the transformation of peritoneal and embryonic cells, and endometrial cell transport. Immune system disorders and surgical scar implantation may also play a role.
Let’s explore these theories in more detail.
Retrograde or reverse menstruation is one of the most widely accepted theories for the cause of endometriosis. This phenomenon is prevalent in 90% of menstruating women and occurs when endometrial tissue flows back through the fallopian tubes into the pelvic cavity instead of exiting the body during menstruation.
When blood containing endometrial tissue flows back into the pelvic cavity, it may adhere to the pelvic walls and organs, triggering endometriosis. These endometrial implants then continue to grow and thicken with each menstrual cycle.
Another potential cause of endometriosis is described by the “induction theory.” According to this theory, unknown substances released by the endometrium in the uterus cause other cells in the body to transform into endometrial cells and grow outside the uterus.
The cells most commonly affected in this process are the peritoneum mesenchymal stem cells, which are located on the inner side of the abdomen and stomach.
Endometriosis often begins during puberty. The embryonic cell transformation hypothesis suggests that increasing estrogen levels during puberty may cause embryonic cells to transform into endometrial-like cells that implant outside the uterus. Embryonic cells are responsible for the earliest stages of human development.
Endometriosis may also be caused by direct transplantation of endometrial cells into organs and tissues outside the uterus, such as the abdominal wall. This can occur during surgical procedures involving the pelvic area, like cesarean delivery (C-section) or hysterectomy, where endometrial cells may attach to the surgical incision.
In some cases, endometrial cells from the uterus may be transported to other areas of the body via blood vessels or the lymphatic system, similar to how cancer cells spread throughout the body.
Recent studies suggest that certain immune system disorders may inhibit the body’s ability to recognize, combat, and destroy endometrial cells that travel outside the uterus. A malfunctioning immune system may allow these cells to implant and thrive in other areas of the body.
Endometriosis can occur at any point during a woman’s reproductive years, but it is more likely to develop after the first menstrual cycle (menarche). Symptoms may take years to become noticeable, and in asymptomatic patients, a diagnosis is often only achieved when investigating unexplained infertility.

While the idiopathic nature of endometriosis makes it challenging to diagnose and treat, certain risk factors may increase your likelihood of developing this condition. Let’s explore these risk factors in detail.
If you have never given birth, you may be at a greater risk of developing endometriosis. Pregnancy temporarily halts the menstrual cycle and lowers estrogen levels, reducing the growth of endometrial cells both inside and outside the uterus. For those with existing endometriosis, pregnancy may temporarily alleviate symptoms.
However, endometriosis can still develop post-pregnancy, often due to the transfer of endometrial cells to other organs during a cesarean section. Postpartum endometriosis may also occur in women who experienced long labor, as the prolonged period between the rupture of the fetal membrane and delivery increases the risk of contamination and infections.
Certain aspects of your menstrual history may increase the likelihood of developing endometriosis, including:
Early menarche and late menopause increase exposure to retrograde menstruation, while heavy or long periods indicate an abundance of endometrial tissue, both of which can contribute to the development of endometriosis.
Endometriosis often begins during puberty, but women in their 20s, 30s, and 40s are more likely to be diagnosed. This increased diagnosis rate may be attributed to attempts to conceive, leading to the discovery of infertility issues.
Genetics may play a role in the prevalence of endometriosis in certain demographics, though no direct correlation has been established. You are at greater risk if one or more of your first-degree relatives (mother, aunts, or sisters) have endometriosis. A family history of infertility may also be a genetic risk factor for developing this condition.
Excessively high levels of estrogen or prolonged exposure to this hormone can increase your risk of endometriosis. Estrogen supports the growth and thickening of the endometrium during the menstrual cycle, which can lead to the buildup of endometrial tissue both inside and outside the uterus.
Women with a slight, smaller frame or low Body Mass Index (BMI) are more likely to develop endometriosis. However, the connection between low BMI and endometriosis is not entirely clear. Interestingly, recent studies have shown that nearly 40% of participants with endometriosis were overweight or obese, suggesting that a high BMI can also be a risk factor.
Certain medical conditions can prevent menstrual blood from flowing out of the body as expected, leading to retrograde menstruation. Conditions that may contribute to this include abnormalities or obstructions in the uterus, vagina, or cervix.
Disorders of the reproductive tract can increase the risk of endometriosis. These include:
Although endometriosis affects up to 11% of women of reproductive age, obtaining an accurate diagnosis can often take nearly seven years. Recent improvements in diagnostic protocols aim to shorten this delay and ensure that women with endometriosis receive timely and appropriate treatment.

Here are some of the tools used to diagnose endometriosis:
Endometriosis is a chronic condition, and its symptoms may sometimes alleviate or disappear on their own, particularly during certain health phases such as pregnancy or menopause. However, in most cases, endometrial growths outside the uterus will continue to proliferate with each menstrual cycle, worsening symptoms over time.
If symptoms become debilitating or life-limiting, a healthcare provider may recommend various treatments to ease pain and improve quality of life. For women of reproductive age, discussing fertility goals with a healthcare provider is essential before choosing a treatment plan for endometriosis.
Below are some of the most commonly recommended treatment options.
Endometrial implants and endometriosis are hormone-dependent. Therefore, hormonal therapies that suppress certain hormones can slow the progression of endometrial implants and alleviate symptoms. Common hormonal therapies include:
When opting for these treatments, it is important to consider your conception plans, as most hormone suppressants will prevent pregnancy.
Over-the-counter pain medications and non-steroidal anti-inflammatory drugs (NSAIDs) can help manage the symptoms of endometriosis by providing temporary relief during flare-ups. However, medications may not be effective for all patients with endometriosis, so other approaches may be considered depending on the assessment of the healthcare provider.
Two common surgical interventions for endometriosis are laparoscopy and hysterectomy:
Although there is no permanent cure for endometriosis, it is important to address this condition with adequate treatment. Without treatment, endometrial implants outside the uterus will continue to grow with each menstrual cycle, potentially leading to severe complications such as:
The World Health Organization estimates that around 10% of women of reproductive age worldwide have endometriosis, accounting for approximately 190 million people globally. The condition is present in nearly 40% of infertile women and is most prevalent among women aged 15 to 44.
While these statistics highlight how common endometriosis is, the actual number of women with the condition may be higher due to underdiagnosis or misdiagnosis. The prevalence of endometriosis can also vary by race and ethnicity.
A 2019 study indicates that Black women are less likely to receive an accurate diagnosis compared to White women, while Asian women are more likely to be diagnosed. Research on the prevalence of endometriosis among other ethnic groups, including American Indian patients, is still limited. On average, women wait between 8 and 12 years from the onset of symptoms to be diagnosed with endometriosis.
When exploring treatments for endometriosis, it’s essential to consider innovative, holistic approaches.
At NextPain Care, our approach to treating endometriosis is grounded in the latest research and guidelines from reputable organizations like the World Health Organization and the American Medical Association. We utilize evidence-based practices, adhering to the highest standards set by leading medical authorities to ensure you receive the best possible care.
We tailor programs to meet each patient’s unique needs and goals, combining various treatments to enhance patients’ quality of life.
Let’s look at this whole-person approach in more detail:
Mindfulness and meditation are techniques used to manage chronic pain by promoting relaxation and mental focus. NextPain Care incorporates these practices into its holistic approach to pain management, helping patients reduce pain perception and improve their...
Nerve blocks involve the injection of medication to interrupt pain signals from specific nerves. NextPain Care uses nerve blocks to provide targeted pain relief for various conditions, including chronic pain and acute post-surgical pain. This minimally...
Radiofrequency ablation is a procedure that uses heat to disable nerves responsible for transmitting pain signals. At NextPain Care, this minimally invasive treatment is utilized to address chronic pain conditions, particularly in the spine. NextPain Care's...
We take great pride in the wealth of talent and expertise that our providers have as they improve the health outcomes of our patients, each and every day.

Your path to understanding and managing endometriosis begins here.